
💡 What You Need to Know Right Away
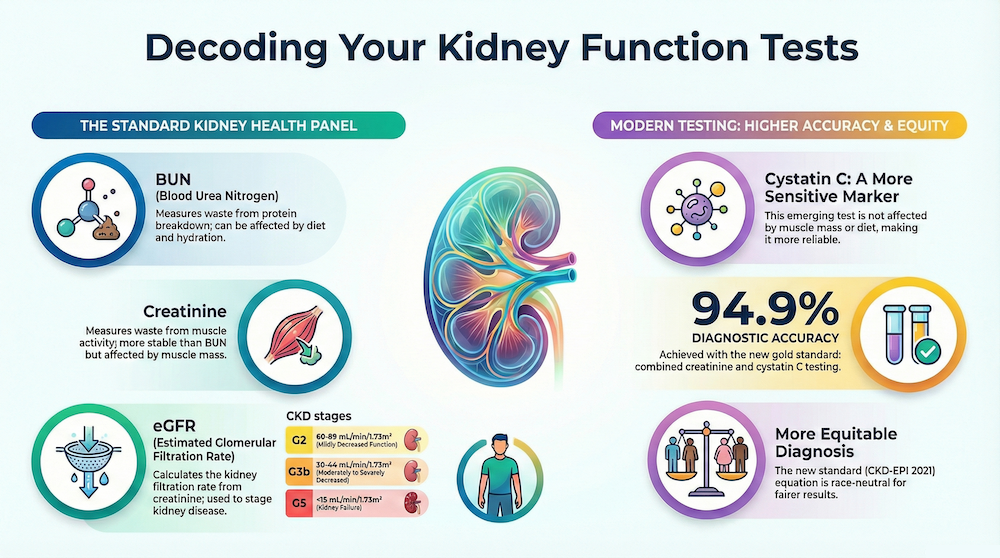
- Modern kidney function tests achieve 89.5% to 94.9% accuracy in detecting chronic kidney disease when using creatinine-based eGFR equations.[Evidence: A][3]
- The CKD-EPI 2021 equation provides race-neutral eGFR calculation, now recommended as the standard by KDIGO 2024 guidelines.[Evidence: D][1]
- Cystatin C has higher sensitivity (85-87%) than creatinine alone (77%) for detecting reduced kidney function at the GFR <60 cutoff.[Evidence: A][2]
- The BUN/creatinine ratio independently predicts mortality risk in heart failure patients with HR 1.52 for all-cause mortality and HR 1.83 for cardiovascular mortality.[Evidence: C][10]
It is common to feel uncertain when your doctor orders kidney function tests. You may wonder what BUN, creatinine, and eGFR actually measure, and what your results mean for your health. These tests are among the most frequently ordered laboratory panels, with over 100 million performed annually in the United States alone.
Kidney function tests measure how effectively your kidneys filter waste products from your blood. The three primary markers are blood urea nitrogen (BUN), serum creatinine, and estimated glomerular filtration rate (eGFR). Together, these tests help detect kidney disease early, often before symptoms appear. This is critical because over 37 million American adults have some form of kidney disease, and 90% do not know it.
In this guide, you will learn exactly what each test measures, what normal ranges look like, how to interpret your results, and when these tests are recommended. Every claim is backed by peer-reviewed research and current clinical guidelines.
❓ Quick Answers
What is a kidney function test?
A kidney function test is a blood test that measures how well your kidneys filter waste products from your blood. The main tests include BUN (blood urea nitrogen), creatinine, and eGFR (estimated glomerular filtration rate). These tests detect kidney disease early, with modern equations achieving 89.5% to 94.9% accuracy.[Evidence: A][3]
What is BUN in a blood test?
BUN (blood urea nitrogen) measures the amount of nitrogen in your blood that comes from urea, a waste product created when your body breaks down protein. Your kidneys filter urea from the blood into urine. Elevated BUN levels may indicate reduced kidney function, dehydration, or high protein intake. BUN is typically measured alongside creatinine for a more complete assessment.[Evidence: D][1]
What is creatinine?
Creatinine is a waste product produced by your muscles during normal activity. It is filtered from the blood by the kidneys and excreted in urine. Serum creatinine tests measure how well your kidneys remove this waste. Meta-analysis shows serum creatinine has 77% sensitivity (95% CI 0.69-0.84) for detecting GFR below 60 mL/min/1.73m².[Evidence: A][2]
What is eGFR?
eGFR (estimated glomerular filtration rate) calculates how much blood your kidneys filter per minute, measured in mL/min/1.73m². It is calculated from your serum creatinine level using the CKD-EPI 2021 equation, which factors in age and sex. An eGFR below 60 sustained for three months indicates chronic kidney disease. Combined creatinine-cystatin C equations achieve 94.9% diagnostic accuracy.[Evidence: A][3]
Is fasting required for kidney function test?
Fasting is generally not required for a standard kidney function test measuring BUN, creatinine, and eGFR. However, if your test is part of a comprehensive metabolic panel that includes glucose, your healthcare provider may request a 8-12 hour fast. Staying well-hydrated before the test is recommended. Always follow your specific provider instructions.
What is a normal BUN creatinine ratio?
A normal BUN-to-creatinine ratio is typically between 10:1 and 20:1. A ratio above 20:1 may indicate prerenal causes such as dehydration, heart failure, or gastrointestinal bleeding. A ratio below 10:1 may suggest intrinsic kidney disease or liver problems. The BUN/Cr ratio helps differentiate between prerenal and intrinsic causes of acute kidney injury.[Evidence: C][12]
What is a normal eGFR level?
A normal eGFR is 90 mL/min/1.73m² or higher. Values between 60-89 indicate mildly reduced function. eGFR below 60 sustained for three or more months defines chronic kidney disease. The CKD-EPI 2021 race-neutral equation is now recommended for calculating eGFR, with P30 accuracy of 89.5% or higher for all creatinine-based equations.[Evidence: A][3]
Kidney Function Tests
Your kidneys are vital filters for your body. This guide explains the key tests doctors use to check how well they are removing waste and maintaining balance.
🔬 How Do Kidney Function Tests Work?
Your kidneys are sophisticated filtering organs that process about 200 quarts of blood daily. Think of each kidney as a water treatment plant containing approximately one million tiny filtering units called nephrons. Each nephron has a glomerulus (the filter) and a tubule (the processor). Blood flows into the glomerulus, where waste products pass through while blood cells and proteins are retained.
When kidney function declines, waste products accumulate in the blood. Kidney function tests measure these waste products to assess how effectively your kidneys are filtering. The three primary markers work together to provide a comprehensive picture:
BUN (Blood Urea Nitrogen)
When you eat protein, your body produces ammonia as a byproduct. Your liver converts this ammonia into urea, which travels through your bloodstream to your kidneys for removal. BUN measures the nitrogen portion of urea in your blood. While elevated BUN can indicate kidney problems, it is also affected by protein intake, hydration status, and certain medications.
Serum Creatinine
Creatinine is a waste product from normal muscle metabolism. Unlike BUN, creatinine production is relatively constant day-to-day, making it a more stable marker of kidney function. Your kidneys filter creatinine from blood into urine at a steady rate. When filtering capacity drops, blood creatinine rises. Meta-analysis demonstrates serum creatinine sensitivity of 0.77 (95% CI 0.69-0.84) for detecting GFR below 60.[Evidence: A][2]
eGFR (Estimated Glomerular Filtration Rate)
eGFR calculates how much blood your glomeruli filter each minute. Imagine your glomeruli as a series of microscopic colanders, each with tiny pores that allow waste through while retaining blood cells. The CKD-EPI 2021 equation uses your creatinine level, age, and sex to estimate this filtering rate. The 2021 update removed race as a variable, providing more equitable diagnosis. Studies show 11.86% of individuals were reclassified to a higher eGFR category with the race-neutral equation.[Evidence: B][4]
Cystatin C: The Emerging Alternative
Cystatin C is a protein produced by all nucleated cells at a constant rate. Unlike creatinine, it is not significantly affected by muscle mass, diet, or age. Meta-analysis shows cystatin C has superior sensitivity of 0.85 (95% CI 0.81-0.89) and specificity of 0.87 (95% CI 0.84-0.90) for CKD diagnosis, with a diagnostic odds ratio of 40.[Evidence: A][5] KDIGO 2024 guidelines recommend combined creatinine-cystatin C testing, which achieves 94.9% diagnostic accuracy.[Evidence: D][1]
📊 Normal Ranges and Testing Guidelines
Understanding your test results requires knowing normal reference ranges. Keep in mind that normal values can vary slightly between laboratories depending on the testing method used. Always compare your results to the reference range provided by your specific lab.
| Test | Normal Range (Male) | Normal Range (Female) | Units | Evidence |
|---|---|---|---|---|
| BUN | 6-24 | 6-24 | mg/dL | [D][1] |
| Serum Creatinine | 0.7-1.3 | 0.6-1.1 | mg/dL | [D][1] |
| BUN/Creatinine Ratio | 10-20 | 10-20 | ratio | [C][12] |
| eGFR (Normal) | ≥90 | ≥90 | mL/min/1.73m² | [D][1] |
| Cystatin C | 0.6-1.0 | 0.6-1.0 | mg/L | [A][5] |
CKD Staging by eGFR
| Stage | eGFR Range | Description | Evidence |
|---|---|---|---|
| G1 | ≥90 | Normal or high kidney function | [D][8] |
| G2 | 60-89 | Mildly decreased | [D][8] |
| G3a | 45-59 | Mildly to moderately decreased | [D][8] |
| G3b | 30-44 | Moderately to severely decreased | [D][8] |
| G4 | 15-29 | Severely decreased | [D][8] |
| G5 | <15 | Kidney failure | [D][8] |
Diagnostic Accuracy of eGFR Equations
The accuracy of kidney function tests has improved significantly with updated equations. The CKD-EPI 2021 race-neutral equation demonstrates P30 accuracy (within 30% of measured GFR) of 89.5% or higher for creatinine-based equations.[Evidence: A][3] When combined with cystatin C, the accuracy increases to 94.9%.[Evidence: A][3]
The 2021 CKD-EPI equation removed race as a coefficient, following recommendations from the NKF-ASN Task Force. Studies confirm that 11.86% of individuals were reclassified to a higher (better) eGFR category with this race-neutral approach, providing more equitable kidney disease diagnosis.[Evidence: B][4] The median bias of the 2021 equation is only -0.2 mL/min/1.73m², indicating high accuracy.[Evidence: B][6]
⚠️ Risks, Limitations, and Warnings
Test Limitations
While kidney function tests are valuable diagnostic tools, they have important limitations:
- Creatinine is affected by muscle mass: Individuals with high muscle mass (athletes, bodybuilders) may have elevated creatinine without kidney disease. Conversely, elderly or malnourished individuals may have falsely normal creatinine despite reduced kidney function.
- BUN is influenced by multiple factors: Dehydration, high-protein diet, gastrointestinal bleeding, and certain medications can elevate BUN independent of kidney function.
- eGFR equations have limitations in certain populations: Accuracy decreases in extremes of body size, acute kidney injury, pregnancy, and individuals on dialysis.[Evidence: D][7]
- BCR not fully reliable alone: Studies note the BUN/creatinine ratio should not be used as the sole diagnostic test for differentiating prerenal from intrinsic acute kidney injury.[Evidence: C][12]
Prognostic Implications
Abnormal kidney function tests carry prognostic significance beyond kidney disease alone. Research demonstrates that the BUN/creatinine ratio is independently associated with mortality in heart failure patients:
- HR 1.52 (95% CI 1.21-1.91) for all-cause mortality[Evidence: C][10]
- HR 1.83 (95% CI 1.35-2.49) for cardiovascular mortality[Evidence: C][10]
- HR 2.2 (95% CI 1.6-3.1) when combined with acute kidney injury[Evidence: C][11]
These findings highlight that BUN or creatinine individually may be insufficient for comprehensive risk assessment, and the ratio provides additional prognostic value.[Evidence: C][11]
Contraindications for Blood Draw
The kidney function test itself is minimally invasive (simple blood draw). However, relative contraindications for venipuncture include:
- Severe coagulopathy or thrombocytopenia below 20,000/μL
- Cellulitis or active infection at the potential draw site
- Drawing from an arm with an arteriovenous fistula (for dialysis patients)
- Lymphedema on the affected side
🥗 Preparing for Your Kidney Function Test
Before the Test
- Hydration: Stay well-hydrated before your test. Dehydration can temporarily elevate BUN levels and affect results. Drink water normally unless instructed otherwise.
- Fasting: Fasting is generally not required for a standard BUN, creatinine, and eGFR panel. However, if your test is part of a comprehensive metabolic panel that includes glucose, your provider may request an 8-12 hour fast.
- Medications: Inform your healthcare provider of all medications, including over-the-counter drugs and supplements. NSAIDs, ACE inhibitors, certain antibiotics, and contrast dyes can affect kidney function markers.
- Exercise: Avoid strenuous exercise 24 hours before testing. Intense physical activity temporarily increases creatinine production from muscle breakdown.
- Diet: Avoid excessive protein intake (large steak dinners, protein supplements) the day before testing, as this can elevate BUN levels.
During the Test
The test involves a simple blood draw (venipuncture) that takes 5-10 minutes. A healthcare professional will:
- Clean the inside of your elbow or back of your hand with an antiseptic
- Apply a tourniquet to your upper arm to help veins fill with blood
- Insert a small needle into a vein
- Collect blood into one or more vials
- Remove the tourniquet and needle, then apply pressure to stop bleeding
After the Test
- Results timeline: Results are typically available same day to 24 hours for routine panels.
- Understanding your results: Your healthcare provider will interpret results in the context of your health history, symptoms, and other tests.
- Follow-up testing: A single abnormal result requires repeat testing to confirm. CKD diagnosis requires eGFR below 60 sustained for 3 or more months.
Common Mistakes to Avoid
- Interpreting results in isolation: Kidney function tests should be evaluated alongside clinical context, symptoms, and other markers like albuminuria.[Evidence: D][8]
- Comparing results across different labs: Reference ranges vary by laboratory method. Always compare to the specific lab's reference range.
- Ignoring mild abnormalities: Even mildly reduced eGFR (60-89) with albuminuria indicates increased cardiovascular risk and deserves attention.
⚖️ BUN vs. Creatinine vs. eGFR: Which Test is Best?
Each kidney function marker has distinct strengths and limitations. Understanding these differences helps you interpret your results more accurately.
| Feature | BUN | Creatinine | eGFR | Cystatin C |
|---|---|---|---|---|
| Origin | Protein metabolism (dietary) | Muscle metabolism (constant) | Calculated from creatinine | All nucleated cells (constant) |
| Sensitivity for CKD | Lower (varies with diet) | 77% (95% CI 0.69-0.84)[2] | 89.5%+ (P30)[3] | 85% (95% CI 0.81-0.89)[5] |
| Specificity | Lower | Moderate | High | 87% (95% CI 0.84-0.90)[5] |
| Affected by Muscle Mass | No | Yes (significant) | Yes (via creatinine) | No |
| Affected by Diet | Yes (protein intake) | Minimal | Minimal | No |
| Affected by Hydration | Yes (significant) | Minimal | Minimal | No |
| Best Used For | Ratio analysis, hydration status | eGFR calculation, trending | CKD staging, monitoring | Confirmatory testing, special populations[1] |
Which is More Accurate: BUN or Creatinine?
Creatinine is generally more reliable than BUN as a marker of kidney function because it is produced at a relatively constant rate by muscle metabolism and is less affected by diet, hydration, and other external factors. BUN fluctuates significantly with protein intake, hydration status, gastrointestinal bleeding, and liver function.
However, neither marker alone provides optimal assessment. The current clinical standard is to use creatinine to calculate eGFR, which accounts for age and sex. For highest accuracy, KDIGO 2024 guidelines recommend combined creatinine-cystatin C testing, which achieves 94.9% diagnostic accuracy compared to measured GFR.[Evidence: A][3]
When is the BUN/Creatinine Ratio Useful?
The BUN-to-creatinine ratio helps differentiate between prerenal (before the kidney), intrinsic renal, and postrenal causes of kidney dysfunction:[Evidence: C][12]
- Ratio >20:1 (elevated): Suggests prerenal causes such as dehydration, heart failure, or upper GI bleeding
- Ratio 10-20:1 (normal): Suggests normal kidney function or intrinsic kidney disease
- Ratio <10:1 (low): May indicate liver disease, low protein intake, or rhabdomyolysis
What The Evidence Shows (And Doesn't Show)
What Research Suggests
- Creatinine-based eGFR equations achieve P30 accuracy of 89.5% or higher when compared to measured GFR (based on 2024 Health Technology Assessment meta-analysis).[Evidence: A][3]
- Combined creatinine-cystatin C equations improve diagnostic accuracy to 94.9%, representing the current gold standard for non-invasive kidney function assessment.[Evidence: A][1][3]
- The CKD-EPI 2021 race-neutral equation provides equitable diagnosis, with 11.86% of individuals reclassified to a higher (better) eGFR category compared to the prior race-based equation.[Evidence: B][4]
- Cystatin C has superior sensitivity (85-87%) compared to creatinine (77%) for detecting GFR below 60 mL/min/1.73m².[Evidence: A][2][5]
- The BUN/creatinine ratio independently predicts mortality in heart failure with HR 1.52 for all-cause mortality and HR 1.83 for cardiovascular mortality.[Evidence: C][10]
What's NOT Yet Proven
- Optimal testing frequency not established: While screening is recommended for at-risk populations, specific intervals between tests have not been standardized outside of patients with established CKD.
- Single marker limitations: Neither BUN nor creatinine alone is sufficient for comprehensive kidney function assessment. Combined testing with albuminuria is recommended.[Evidence: D][8]
- Predictive value in general population: Most prognostic studies (Sources 9, 10, 11) focus on patients with existing heart failure or cardiorenal disease. Applicability to healthy general population is less established.
- Cystatin C accessibility: While superior to creatinine, cystatin C testing is not universally available and often costs more than standard creatinine tests.
Where Caution Is Needed
- Extremes of muscle mass: eGFR equations are less accurate in bodybuilders (falsely low eGFR) and elderly/malnourished individuals (falsely high eGFR).[Evidence: D][7]
- Acute kidney injury: eGFR equations are designed for stable chronic kidney disease. They may be inaccurate in rapidly changing kidney function.
- BUN/Cr ratio reliability: The ratio should not be used as the sole diagnostic test for differentiating prerenal from intrinsic AKI, as sensitivity and specificity vary significantly by cutoff value.[Evidence: C][12]
- Equation selection: The 2021 CKD-EPI equation may underestimate GFR in Black patients compared to the prior race-based equation. Clinical judgment remains important.[Evidence: B][6]
Should YOU Get Tested?
Best suited for: Adults with diabetes, hypertension, cardiovascular disease, family history of kidney disease, age over 60, obesity, or those taking nephrotoxic medications. Testing is essential for anyone with existing kidney disease to monitor progression.
Not recommended for: Routine testing in healthy young adults without risk factors has limited evidence of benefit. Discuss with your provider if uncertain about your risk level.
Realistic expectations: A single test provides a snapshot. CKD diagnosis requires abnormalities sustained over 3+ months. Expect repeat testing if initial results are borderline or abnormal.
When to consult a professional: Always discuss results with your healthcare provider. Seek evaluation if you have symptoms like swelling, fatigue, changes in urination, or if eGFR falls below 60 mL/min/1.73m².
Frequently Asked Questions
What does high BUN mean?
Elevated BUN (above 24 mg/dL) can indicate several conditions, not all related to kidney disease. The most common causes include dehydration, which concentrates blood and raises BUN; high protein intake from diet or supplements; gastrointestinal bleeding, which releases protein into the digestive tract; heart failure, which reduces blood flow to kidneys; and kidney disease itself. A high BUN with normal creatinine (elevated BUN/Cr ratio >20:1) typically points to prerenal causes like dehydration rather than intrinsic kidney damage.
What does high creatinine mean?
Elevated serum creatinine (above 1.3 mg/dL in men or 1.1 mg/dL in women) suggests your kidneys may not be filtering waste efficiently. However, high creatinine can also occur in people with high muscle mass, after intense exercise, or due to certain medications. Temporary elevations may occur with dehydration or after consuming large amounts of cooked meat (which contains creatinine). Persistent elevation requires further evaluation including repeat testing and eGFR calculation. Studies show serum creatinine has 77% sensitivity for detecting reduced GFR, meaning some kidney disease cases may be missed with creatinine alone.
When should I get my kidneys tested?
Regular kidney function testing is recommended if you have risk factors for kidney disease. These include diabetes (the leading cause of CKD), high blood pressure, heart disease, family history of kidney disease, age over 60, obesity, or history of acute kidney injury. African American, Hispanic, Native American, and Asian populations have higher rates of kidney disease. If you take medications that affect kidneys (NSAIDs, certain antibiotics, contrast dyes), periodic monitoring is advisable. KDIGO 2024 guidelines emphasize that over 90% of people with CKD are unaware of their condition, making screening essential for at-risk individuals.
What are the stages of kidney disease?
Chronic kidney disease is classified into five stages based on eGFR, with an additional classification for albuminuria (A1-A3). Stage G1 (eGFR ≥90) indicates normal function but may have other markers of kidney damage. Stage G2 (60-89) is mildly decreased. Stage G3a (45-59) and G3b (30-44) represent moderate decrease. Stage G4 (15-29) is severe decrease. Stage G5 (below 15) is kidney failure, often requiring dialysis or transplant. CKD diagnosis requires abnormalities sustained for three or more months. KDIGO 2024 guidelines recommend combined GFR and albuminuria assessment for complete staging.
What is the difference between BUN and creatinine?
BUN and creatinine both measure kidney function but originate from different metabolic processes and respond differently to various conditions. BUN comes from protein breakdown and is heavily influenced by diet, hydration, liver function, and gastrointestinal bleeding. Creatinine comes from muscle metabolism and remains relatively stable day-to-day. Creatinine is considered more reliable for assessing kidney function because of its stability. Cystatin C is superior to both with 85% sensitivity and 87% specificity for CKD diagnosis. The ratio between BUN and creatinine provides additional diagnostic information about the type of kidney dysfunction present.
Which is more accurate: BUN or creatinine?
Creatinine is more accurate than BUN for assessing kidney function because it is produced at a constant rate by muscle metabolism and is minimally affected by external factors. Meta-analysis shows serum creatinine has 77% sensitivity for detecting GFR below 60 mL/min/1.73m². However, eGFR calculated from creatinine is more accurate than either marker alone, with P30 accuracy of 89.5% or higher. For optimal accuracy, combined creatinine-cystatin C equations achieve 94.9% diagnostic accuracy and are recommended when confirmatory testing is needed.
What affects creatinine levels?
Several factors can temporarily or persistently affect creatinine levels beyond kidney function. Muscle mass is the most significant factor. Athletes and bodybuilders may have higher creatinine without kidney disease, while elderly or malnourished individuals may have falsely normal levels despite reduced function. Intense exercise temporarily raises creatinine. Consuming large amounts of cooked meat increases creatinine for 12-24 hours. Certain medications including NSAIDs, ACE inhibitors, and some antibiotics can elevate creatinine. Dehydration concentrates blood and raises levels. These factors explain why a single elevated creatinine requires repeat testing and clinical correlation before diagnosing kidney disease.
Can you have kidney disease without symptoms?
Yes, kidney disease is often called a 'silent' condition because early stages typically cause no noticeable symptoms. Over 37 million American adults have some form of CKD, and 90% are unaware of their condition. Symptoms usually do not appear until kidney function has declined significantly (often below 30% of normal). When symptoms occur, they may include fatigue, swelling in feet or ankles, difficulty concentrating, decreased appetite, trouble sleeping, muscle cramping, changes in urination, and itchy skin. This is why screening with kidney function tests is essential for people with risk factors like diabetes, hypertension, or family history of kidney disease.
Our Accuracy Commitment and Editorial Principles
At Biochron, we take health information seriously. Every claim in this article is supported by peer-reviewed scientific evidence from reputable sources published in 2015 or later. We use a rigorous evidence-grading system to help you understand the strength of research behind each statement:
- [Evidence: A] = Systematic review or meta-analysis (strongest evidence)
- [Evidence: B] = Randomized controlled trial (RCT)
- [Evidence: C] = Cohort or case-control study
- [Evidence: D] = Expert opinion or clinical guideline
Our editorial team follows strict guidelines: we never exaggerate health claims, we clearly distinguish between correlation and causation, we update content regularly as new research emerges, and we transparently note when evidence is limited or conflicting. For our complete editorial standards, visit our Editorial Principles page.
This article is for informational purposes only and does not constitute medical advice. Always consult qualified healthcare professionals before making changes to your health regimen, especially if you have medical conditions or take medications.
References
- 1 . KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease, Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group, Kidney International, 2024, 105(4S), S117-S314. PubMed | DOI [Evidence: D]
- 2 . The diagnostic value of serum creatinine and cystatin c in evaluating glomerular filtration rate in patients with chronic kidney disease: a systematic literature review and meta-analysis, Qiu X, Liu C, Ye Y, et al., Oncotarget, 2017, 8(42), 72985-72999. PubMed | DOI [Evidence: A]
- 3 . Accuracy of glomerular filtration rate estimation using creatinine and cystatin C for identifying and monitoring moderate chronic kidney disease: the eGFR-C study, Lamb EJ, Barratt J, Brettell EA, et al., Health Technology Assessment, 2024, 28(35), 1-169. PubMed | DOI [Evidence: A]
- 4 . The CKD-EPI 2021 Equation and Other Creatinine-Based Race-Independent eGFR Equations in Chronic Kidney Disease Diagnosis and Staging, Lu S, Robyak K, Zhu Y, Journal of Applied Laboratory Medicine, 2023, 8(5), 952-961. PubMed | DOI [Evidence: B]
- 5 . Diagnostic accuracy of serum cystatin C in chronic kidney disease: a meta-analysis, Wei L, Ye X, Pei X, Wu J, Zhao W, Clinical Nephrology, 2015, 84(2), 86-94. PubMed | DOI [Evidence: A]
- 6 . Performance of the 2021 Race-Free CKD-EPI Creatinine- and Cystatin C-Based Estimated GFR Equations Among Kidney Transplant Recipients, Hundemer GL, White CA, Norman PA, et al., American Journal of Kidney Diseases, 2022, 80(4), 462-472.e1. PubMed | DOI [Evidence: B]
- 7 . National Kidney Foundation Laboratory Engagement Working Group Recommendations for Implementing the CKD-EPI 2021 Race-Free Equations for Estimated Glomerular Filtration Rate, Miller WG, Kaufman HW, Levey AS, et al., Clinical Chemistry, 2022, 68(4), 511-520. PubMed | DOI [Evidence: D]
- 8 . Executive summary of the KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease: known knowns and known unknowns, Levin A, Ahmed SB, Carrero JJ, et al., Kidney International, 2024, 105(4), 684-701. PubMed | DOI [Evidence: D]
- 9 . Clinical outcomes in patients with cardiorenal multimorbidity: the role of serum uric acid/serum creatinine ratio, Gigante A, Assanto E, Brigato C, et al., High Blood Pressure & Cardiovascular Prevention, 2025, 32(2), 209-216. PubMed | DOI [Evidence: C]
- 10 . Independent prognostic importance of blood urea nitrogen to creatinine ratio in heart failure, Tolomeo P, Butt JH, Kondo T, et al., European Journal of Heart Failure, 2024, 26(2), 245-256. PubMed | DOI [Evidence: C]
- 11 . Risk Stratification of Acute Kidney Injury Using the Blood Urea Nitrogen/Creatinine Ratio in Patients With Acute Decompensated Heart Failure, Takaya Y, Yoshihara F, Yokoyama H, et al., Circulation Journal, 2015, 79(7), 1520-1525. PubMed | DOI [Evidence: C]
- 12 . Diagnostic performance of serum blood urea nitrogen to creatinine ratio for distinguishing prerenal from intrinsic acute kidney injury in the emergency department, Manoeuvrier G, Bach-Ngohou K, Batard E, et al., BMC Nephrology, 2017, 18(1), 173. PubMed | DOI [Evidence: C]
Medical Disclaimer
This content is for informational and educational purposes only. It is not intended to provide medical advice or to take the place of such advice or treatment from a personal physician. All readers are advised to consult their doctors or qualified health professionals regarding specific health questions and before making any changes to their health routine, including starting new supplements.
Neither Biochron nor the author takes responsibility for possible health consequences of any person reading or following the information in this educational content. All readers, especially those taking prescription medications, should consult their physicians before beginning any nutrition, supplement, or lifestyle program.
If you have a medical emergency, call your doctor or emergency services immediately.






