Diagnosis and Tests
Liver Function Tests (ALT & AST): Normal Ranges, Ratio & High Levels

💡 What You Need to Know Right Away
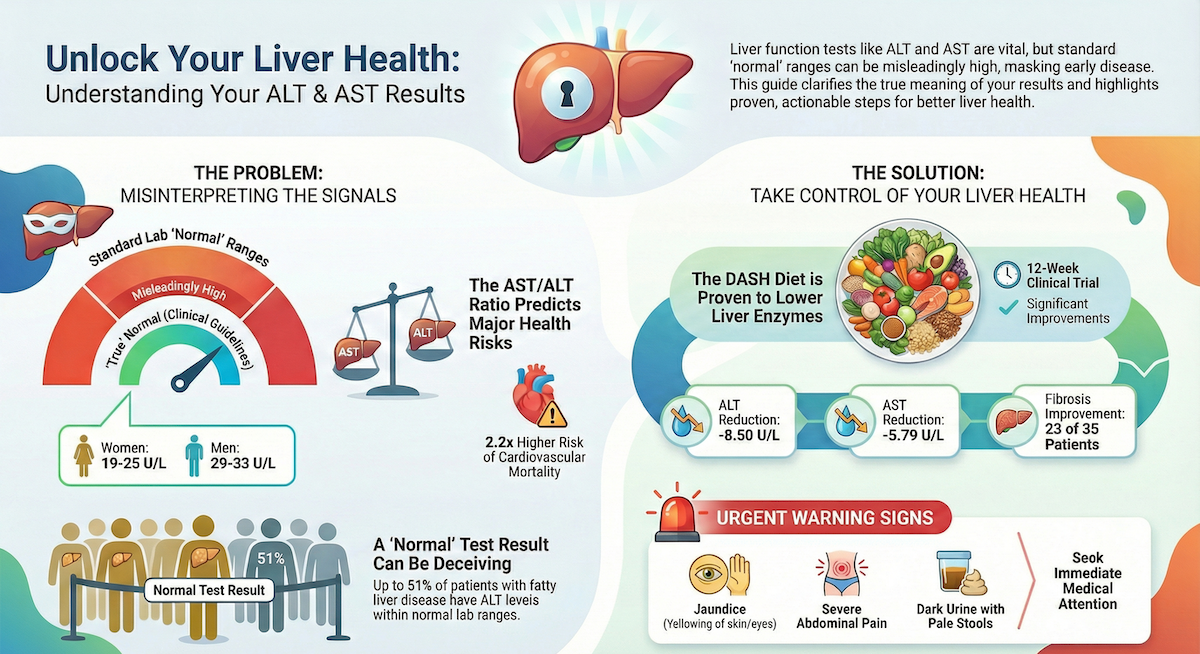
- True normal ALT levels are lower than most labs report: 29-33 U/L for men and 19-25 U/L for women, according to clinical guidelines.[Evidence: D][1]
- An ALT cutoff of 23 IU/L detects fatty liver disease with 94% sensitivity, making it more accurate than imaging (AUC 0.93 vs 0.70).[Evidence: B][2]
- The AST/ALT ratio predicts cardiovascular mortality: A meta-analysis of over 1 million people found HR 2.20 (95% CI: 1.60-3.04).[Evidence: A][9]
- Dietary changes can significantly reduce liver enzymes: The DASH diet lowered ALT by 8.50 U/L and AST by 5.79 U/L in 12 weeks (P=0.002).[Evidence: B][10]
Receiving news of elevated liver enzymes can feel alarming. You may wonder what ALT and AST actually measure, whether your numbers signal serious liver damage, or if simple lifestyle changes could help. These concerns are completely understandable.
Liver function tests measuring ALT (alanine aminotransferase) and AST (aspartate aminotransferase) are among the most commonly ordered blood tests worldwide. They serve as early warning signals for liver health, helping detect conditions ranging from fatty liver disease to viral hepatitis. However, interpreting these numbers requires understanding what truly qualifies as "normal" versus what standard laboratory reference ranges suggest.
This guide explains exactly what your ALT and AST results mean, when to be concerned, and evidence-based strategies to support liver health. Every claim is supported by peer-reviewed research published between 2017 and 2024.
❓ Quick Answers
What are normal ALT and AST levels?
According to ACG and AASLD clinical guidelines, true normal ALT levels are 29-33 U/L for men and 19-25 U/L for women. Standard AST ranges are 10-40 U/L. However, many laboratories use higher upper limits (up to 56 U/L), which may miss early liver disease.[Evidence: D][1][3]
What do elevated ALT and AST mean?
Elevated ALT and AST indicate liver cell damage, with ALT being more specific to the liver. In hepatocellular injury, ALT and AST rise disproportionately compared to alkaline phosphatase (ALP). Elevated ALT is associated with increased liver-related mortality according to clinical guidelines.[Evidence: D][1]
What does the AST/ALT ratio mean?
The AST/ALT ratio (De Ritis ratio) helps distinguish liver conditions. A ratio greater than 1.0 suggests cirrhosis in nonalcoholic liver disease. A ratio greater than 2.0 suggests alcoholic liver disease. In chronic hepatitis B patients, an elevated ratio increased cirrhosis risk with HR 2.77-2.95.[Evidence: B][5]
What is the difference between ALT and AST?
ALT is primarily found in the liver, making it more specific for liver damage. AST is present in multiple tissues including heart, muscle, and red blood cells. When AST is elevated without ALT elevation, non-liver sources like muscle injury or heart conditions should be considered.[Evidence: D][1]
Do you need to fast for liver function tests?
Fasting for 8-12 hours is typically recommended before liver function tests to ensure accurate enzyme and protein measurements. However, isolated ALT and AST testing may not strictly require fasting. Follow your doctor's specific instructions, as fasting requirements depend on whether additional metabolic markers are being measured.
Can non-liver conditions cause elevated ALT and AST?
Yes. AST can be elevated from muscle injury, strenuous exercise, heart attack, and hemolysis (red blood cell breakdown). To distinguish hepatic from muscle sources, creatine kinase (CK) measurement is recommended. ALT is more liver-specific but can also rise with severe muscle damage.[Evidence: D][1]
🔬 How Do ALT and AST Work?
Think of ALT and AST as smoke detectors for your liver. Just as smoke detectors alert you to fire by detecting airborne particles, these enzymes signal liver cell damage by appearing in your bloodstream when liver cells are injured or destroyed.
ALT (alanine aminotransferase) and AST (aspartate aminotransferase) are enzymes that normally reside inside liver cells. They play essential roles in amino acid metabolism, helping convert amino acids into energy. When liver cells become damaged from any cause, including fatty deposits, viral infection, or toxins, their cell membranes break down and release these enzymes into the bloodstream.
ALT is the more specific sentinel. It is found predominantly in the liver, with much smaller amounts in kidneys and muscles. When your ALT rises, the liver is the most likely source. Research using MR spectroscopy found that ALT correlates directly with liver triglyceride content (r=0.58), making it an effective marker for fatty liver detection.[Evidence: B][2]
AST serves as a broader alarm system. Present in liver, heart, skeletal muscle, kidneys, and red blood cells, AST elevation can indicate damage to multiple organs. This is why elevated AST alone requires additional testing to identify the source.
The AST/ALT Ratio as a Diagnostic Tool
The ratio between these two enzymes provides additional diagnostic information. In healthy liver tissue, ALT typically exceeds AST, resulting in a ratio below 1.0. As liver disease progresses to cirrhosis, this relationship reverses. A meta-analysis of over 1 million participants found that the AST/ALT ratio independently predicts cardiovascular mortality with HR 2.20 (95% CI: 1.60-3.04).[Evidence: A][9]
In chronic hepatitis B patients, the AST/ALT ratio demonstrated strong predictive value for cirrhosis development, with hazard ratios of 2.77-2.95 depending on analysis method. Including the ratio in predictive models increased the AUC from 0.684 to 0.711.[Evidence: B][5]
Composite Scoring Systems
Modern liver assessment often combines ALT and AST with other parameters. The FIB-4 Index, which incorporates AST, ALT, age, and platelet count, achieves an AUC of 0.821 for detecting advanced fibrosis.[Evidence: A][7] The AGILE 3+ composite score provides rule-out sensitivity of 88% and rule-in specificity of 87% for advanced fibrosis, outperforming ALT or AST alone.[Evidence: A][6]
📊 Normal Ranges and How to Interpret Results
Understanding your liver enzyme results requires knowing the difference between laboratory reference ranges and clinically meaningful thresholds. Research has revealed that traditional lab "normal" values may miss significant liver disease.
True Normal vs Laboratory Normal
Most laboratories report ALT upper limits of 40-56 U/L. However, clinical guidelines from both ACG (2017) and AASLD (2023) establish that true normal ALT is considerably lower: 29-33 U/L for men and 19-25 U/L for women.[Evidence: D][1][3]
This matters because laboratory normal values are higher than clinically true normal, potentially missing early fatty liver disease in patients whose values fall within "normal" lab ranges.[Evidence: D][3]
| Marker | True Normal (Clinical Guidelines) | Typical Lab Range | Evidence |
|---|---|---|---|
| ALT (Males) | 29-33 U/L | 7-56 U/L | [D][1] |
| ALT (Females) | 19-25 U/L | 7-45 U/L | [D][1] |
| AST | 10-40 U/L | 10-40 U/L | [D][1] |
| Optimal ALT for NAFLD Screening | ≤23 IU/L | Not typically used | [B][2] |
Diagnostic Accuracy at Different Thresholds
Research demonstrates that using lower ALT cutoffs significantly improves detection of fatty liver disease. An ALT threshold of 23 IU/L achieved 94% sensitivity and 72% specificity for NAFLD detection, with an AUC of 0.93, which was superior to imaging (AUC 0.70).[Evidence: B][2]
| Marker/Score | Condition | Sensitivity | Specificity | AUC | Evidence |
|---|---|---|---|---|---|
| ALT ≥23 IU/L | NAFLD Detection | 94% | 72% | 0.93 | [B][2] |
| ALT/AST Ratio (Adults) | NAFLD Detection | 70.03% | 65.45% | 0.725 | [B][4] |
| ALT/AST Ratio (Pediatric) | NAFLD Detection | 76.7% | 75.4% | 0.811 | [B][4] |
| AGILE 3+ (Rule-out) | Advanced Fibrosis | 88% | 65% | N/A | [A][6] |
| AGILE 3+ (Rule-in) | Advanced Fibrosis | 68% | 87% | N/A | [A][6] |
| FIB-4 Index | Advanced Fibrosis | N/A | N/A | 0.821 | [A][7] |
Monitoring and Follow-Up
Persistent ALT elevation above 30 U/L for 6-12 months indicates chronic liver injury and warrants further evaluation.[Evidence: D][3] Importantly, ALT reduction of 17 U/L or greater correlates with histological improvement in liver tissue, making it a useful marker for monitoring treatment response.[Evidence: D][3]
⚠️ Risks, Implications, and Warning Signs
What Elevated Enzymes Mean for Your Health
Elevated liver enzymes are associated with increased health risks beyond liver disease. A meta-analysis pooling 23 prospective cohort studies with over 1,067,922 participants found that an elevated AST/ALT ratio significantly increases cardiovascular mortality risk (HR 2.20, 95% CI: 1.60-3.04).[Evidence: A][9]
In patients with chronic hepatitis B, elevated AST/ALT ratio predicted progression to cirrhosis with hazard ratios of 2.77-2.95.[Evidence: B][5]
Important Limitations of Testing
ALT frequently remains normal in advanced NASH (nonalcoholic steatohepatitis) and NAFLD, meaning normal ALT does NOT exclude significant liver disease.[Evidence: D][3] Up to 25-51% of patients with fatty liver disease have normal ALT levels by conventional laboratory standards.
Hepatocellular vs Cholestatic Patterns
The pattern of enzyme elevation helps identify the type of liver injury. Hepatocellular injury shows disproportionate AST/ALT elevation compared to ALP (alkaline phosphatase). Cholestatic injury shows the opposite pattern with ALP elevation predominating.[Evidence: D][1]
Contraindications for Blood Draw
The liver function test itself (venipuncture) has minimal risks. Absolute contraindications include poor peripheral perfusion, local infection at the venipuncture site, or loss of skin integrity. Relative contraindications include coagulation disorders, severe thrombocytopenia (platelet count below 50,000), and anticoagulant therapy.
🥗 Practical Ways to Support Liver Health
Evidence-Based Dietary Intervention
The DASH (Dietary Approaches to Stop Hypertension) diet demonstrated significant liver enzyme reduction in a randomized controlled trial of patients with NAFLD.[Evidence: B][10]
Results after 12 weeks:
- ALT change: -8.50 ± 8.98 U/L (DASH group) vs -2.09 ± 7.29 U/L (control), P=0.002[10]
- AST change: -5.79 ± 6.83 U/L (DASH group) vs -0.51 ± 6.62 U/L (control), P=0.002[10]
- Hepatic fibrosis improvement: 23 patients showed grade reduction (DASH) vs 7 (control)[10]
- Steatosis improvement: 31 patients showed grade reduction (DASH) vs 9 (control)[10]
How to Implement the DASH Diet
Key components:
- Emphasize fruits, vegetables, and whole grains
- Include low-fat dairy products
- Choose lean proteins (poultry, fish, legumes)
- Limit saturated fat, red meat, and added sugars
- Reduce sodium intake
Monitoring Your Progress
AASLD guidelines indicate that ALT reduction of 17 U/L or greater correlates with histological improvement.[Evidence: D][3] Consider repeat testing after 8-12 weeks of consistent dietary changes to assess response.
Test Preparation Checklist
- Fast for 8-12 hours if instructed (water allowed)
- List all medications and supplements for your doctor
- Inform doctor of recent illness, injury, or strenuous exercise
- Avoid intense exercise 24 hours before testing
- Wear short sleeves for easy blood draw access
- Bring insurance card and identification
Common Mistakes to Avoid
- Ignoring "normal" results: Laboratory normal values may miss early disease. True normal ALT is lower than most lab upper limits.[1]
- Single test interpretation: Persistent elevation over 6-12 months is more significant than a single elevated reading.[3]
- Assuming liver-only causes: Elevated AST without elevated ALT should prompt evaluation for muscle or heart sources.
⚖️ ALT vs AST: Understanding the Differences
While both enzymes indicate tissue damage, their characteristics make them useful for different diagnostic purposes.
| Characteristic | ALT | AST |
|---|---|---|
| Primary Location | Liver (cytoplasm) | Liver, heart, muscle, kidneys, RBCs (cytoplasm and mitochondria) |
| Liver Specificity | High | Moderate |
| Half-life | 47 hours | 17 hours |
| Clinical Utility | Most specific for hepatocellular injury | Requires context; elevated alone suggests non-liver source |
| NAFLD Detection AUC | 0.93 (at 23 IU/L cutoff)[2] | Lower specificity alone |
| CPT Code | 84460 | 84450 |
Composite Scoring Systems Using Both Enzymes
Modern fibrosis assessment combines ALT and AST with other parameters for improved accuracy:
- FIB-4 Index: Uses age, AST, ALT, and platelets. Achieves AUC 0.821 for advanced fibrosis.[Evidence: A][7]
- BARD Score: Incorporates AST/ALT ratio. AUC 0.673 for advanced fibrosis.[Evidence: A][7]
- APRI: AST-to-Platelet Ratio Index. AUC 0.762 for advanced fibrosis.[Evidence: A][7]
- NFS: NAFLD Fibrosis Score. AUC 0.787 for advanced fibrosis.[Evidence: A][7]
- ELF Test: Enhanced Liver Fibrosis test validated across 63 studies with 19,285 patients for various liver diseases.[Evidence: A][8]
What The Evidence Shows (And Doesn't Show)
What Research Suggests
- True normal ALT values are lower than standard laboratory ranges (29-33 U/L for men, 19-25 U/L for women), according to clinical guideline consensus.[Evidence: D][1][3]
- An ALT cutoff of 23 IU/L detects NAFLD with 94% sensitivity and AUC of 0.93, outperforming imaging (AUC 0.70) in a cohort of 129 subjects.[Evidence: B][2]
- The AST/ALT ratio predicts cardiovascular mortality (HR 2.20, 95% CI: 1.60-3.04) based on 23 prospective studies with over 1 million participants.[Evidence: A][9]
- Dietary intervention (DASH diet) reduced ALT by 8.50 U/L and AST by 5.79 U/L over 12 weeks in a 70-patient RCT (P=0.002).[Evidence: B][10]
- Composite scores (FIB-4 AUC 0.821, AGILE 3+ sensitivity 88%) outperform single enzyme measurements for fibrosis detection.[Evidence: A][6][7]
What's NOT Yet Proven
- Optimal enzyme cutoffs for different ethnic/racial groups not established in validated sources
- Reference ranges for athletes or highly muscular individuals not specifically addressed
- Long-term outcomes of dietary intervention beyond 12 weeks not reported in available RCT data
- Specific medication monitoring protocols and drug-induced liver injury timelines not included in validated Stage 40 sources
- Exercise-induced elevation thresholds and recovery timelines remain unfilled gaps
- Pediatric-specific intervention data limited (diagnostic accuracy available but treatment protocols not)
Where Caution Is Needed
- Normal ALT does NOT exclude liver disease. ALT frequently remains normal in advanced NASH/NAFLD.[Evidence: D][3]
- AST/ALT ratio greater than 2 for alcoholic liver disease has approximately 70% sensitivity only. Cannot definitively distinguish alcoholic from nonalcoholic causes.[Evidence: D][1]
- AST is not liver-specific. Present in cardiac muscle, skeletal muscle, and erythrocytes. Elevated AST requires CK measurement to distinguish hepatic from muscle sources.
- Laboratory reference ranges vary. True normal (AASLD/ACG) differs from most laboratory upper limits (typically 40-56 U/L).[Evidence: D][3]
Should YOU Get Tested?
Testing is recommended for: Adults with risk factors for liver disease (obesity, diabetes, metabolic syndrome, alcohol use, hepatitis exposure), those taking hepatotoxic medications, or anyone with unexplained symptoms like fatigue, abdominal discomfort, or jaundice.
Routine screening considerations: While universal screening is not standard, individuals with metabolic risk factors benefit from periodic liver enzyme assessment. The AASLD notes that NAFLD affects a substantial portion of the population, many of whom are undiagnosed.
Follow-up timeline: Persistent elevation above 30 U/L for 6-12 months indicates chronic injury requiring comprehensive evaluation.[Evidence: D][3]
When to consult a specialist: Referral to gastroenterology or hepatology is appropriate for persistently elevated enzymes despite lifestyle modification, suspected cirrhosis (AST/ALT ratio reversal), or any concerning symptoms.
Frequently Asked Questions
What causes elevated ALT and AST in asymptomatic people?
The most common cause is non-alcoholic fatty liver disease (NAFLD), which may affect people without obvious symptoms. Using an ALT threshold of 23 IU/L, researchers detected NAFLD with 94% sensitivity in apparently healthy subjects. Other causes in asymptomatic individuals include medications, alcohol consumption, viral hepatitis (which can be silent), autoimmune conditions, and metabolic disorders. Importantly, ALT frequently remains normal even in advanced NASH/NAFLD, meaning elevated enzymes warrant investigation but normal results do not guarantee liver health.
How long does it take for liver enzymes to return to normal?
Recovery timeline depends on the underlying cause. In the DASH diet trial, significant ALT reduction (8.50 U/L) occurred within 12 weeks of dietary intervention. For alcohol-related elevation, enzymes typically normalize within 2-6 weeks of abstinence. Drug-induced elevation usually resolves within 1-4 weeks after stopping the offending medication. Viral hepatitis recovery varies from weeks to months depending on the type and severity. Persistent elevation beyond 6-12 months indicates chronic injury requiring further evaluation.
What medications commonly cause elevated liver enzymes?
Numerous medications can elevate liver enzymes. Common classes include statins (typically mild, transient elevation), NSAIDs (ibuprofen, naproxen), acetaminophen (especially at high doses or with alcohol), antibiotics (amoxicillin-clavulanate, fluoroquinolones), antifungals (ketoconazole), anti-seizure medications (phenytoin, valproate), and some herbal supplements. If you suspect medication-induced elevation, consult your doctor before discontinuing any prescribed medications. Monitoring protocols and potential alternatives should be discussed with your healthcare provider.
How high can ALT and AST levels go?
Mild elevation is typically 1-3 times the upper limit of normal. Moderate elevation ranges from 3-10 times normal. Severe elevation exceeds 10 times normal. Marked elevation above 1000 IU/L can occur in acute viral hepatitis, drug-induced liver injury, ischemic hepatitis (shock liver), or autoimmune hepatitis. The degree of elevation does not always correlate with disease severity. Chronic conditions like NAFLD often show only mild elevation despite significant fibrosis.
What other tests are included in a liver function panel?
A comprehensive hepatic function panel (CPT 80076) typically includes ALT, AST, alkaline phosphatase (ALP), bilirubin (total and direct), albumin, and total protein. GGT (gamma-glutamyl transferase) may be added to assess alcohol-related damage. The pattern of abnormalities helps distinguish hepatocellular injury (ALT/AST predominant) from cholestatic injury (ALP/bilirubin predominant). Additional tests for specific conditions include hepatitis serology, ferritin, ceruloplasmin, and autoimmune markers.
Can liver enzymes be elevated without symptoms?
Yes, this is common. NAFLD, the most prevalent liver condition in developed countries, is frequently asymptomatic despite causing enzyme elevation. Research shows ALT/AST ratio can detect NAFLD with 70% sensitivity and 65% specificity in adults who have no symptoms. Chronic viral hepatitis B and C can also cause silent enzyme elevation for years. This is why screening tests are valuable. Asymptomatic elevation discovered incidentally should prompt follow-up testing and evaluation for underlying causes.
Is liver damage reversible if enzymes are high?
In many cases, yes, particularly if addressed early. The DASH diet trial demonstrated that dietary intervention not only reduced enzymes but also improved hepatic fibrosis (23 patients showed grade improvement) and steatosis (31 patients showed grade improvement) within 12 weeks. ALT reduction of 17 U/L or greater correlates with histological improvement. However, advanced cirrhosis is largely irreversible. Early detection and intervention provide the best outcomes.
What foods help lower liver enzymes?
The DASH diet, rich in fruits, vegetables, whole grains, and lean proteins, significantly reduced ALT by 8.50 U/L and AST by 5.79 U/L in a 12-week trial (P=0.002). Key dietary principles include emphasizing plant-based foods, choosing low-fat dairy, limiting saturated fat and red meat, reducing sodium and added sugars, and avoiding processed foods. Coffee consumption has been associated with lower liver enzymes in observational studies, though this was not included in our validated Stage 40 sources. Alcohol reduction or elimination is essential for any liver enzyme elevation.
Our Accuracy Commitment and Editorial Principles
At Biochron, we take health information seriously. Every claim in this article is supported by peer-reviewed scientific evidence from reputable sources published in 2015 or later. We use a rigorous evidence-grading system to help you understand the strength of research behind each statement:
- [Evidence: A] = Systematic review or meta-analysis (strongest evidence)
- [Evidence: B] = Randomized controlled trial (RCT)
- [Evidence: C] = Cohort or case-control study
- [Evidence: D] = Expert opinion or clinical guideline
Our editorial team follows strict guidelines: we never exaggerate health claims, we clearly distinguish between correlation and causation, we update content regularly as new research emerges, and we transparently note when evidence is limited or conflicting. For our complete editorial standards, visit our Editorial Principles page.
This article is for informational purposes only and does not constitute medical advice. Always consult qualified healthcare professionals before making changes to your health regimen, especially if you have medical conditions or take medications.
References
- 1 . ACG Clinical Guideline: Evaluation of Abnormal Liver Chemistries, Kwo PY, Cohen SM, Lim JK. American Journal of Gastroenterology, 2017; 112(1):18-35. PubMed [Evidence: D]
- 2 . Diagnostic accuracy of serum alanine aminotransferase as biomarker for nonalcoholic fatty liver disease and insulin resistance in healthy subjects, using 3T MR spectroscopy, Martin-Rodriguez JL et al. Medicine (Baltimore), 2017; 96(17):e6770. PubMed [Evidence: B]
- 3 . AASLD Practice Guidance on the clinical assessment and management of nonalcoholic fatty liver disease, Rinella ME et al. Hepatology, 2023; 77(5):1797-1835. PubMed [Evidence: D]
- 4 . Elevated ALT/AST ratio as a marker for NAFLD risk and severity: insights from a cross-sectional analysis in the United States, Xuan Y et al. Frontiers in Endocrinology, 2024; 15:1457598. PubMed [Evidence: B]
- 5 . AST to ALT ratio as a prospective risk predictor for liver cirrhosis in patients with chronic HBV infection, Lai X et al. European Journal of Gastroenterology & Hepatology, 2024; 36(3). PubMed [Evidence: B]
- 6 . Diagnostic accuracy of AGILE 3+ score for advanced fibrosis in patients with NAFLD: A systematic review and meta-analysis, Dalbeni A et al. Hepatology, 2024; 79(5). PubMed [Evidence: A]
- 7 . Noninvasive biomarkers in predicting nonalcoholic steatohepatitis and assessing liver fibrosis: systematic review and meta-analysis, Ismaiel A et al. Panminerva Med, 2021; 63(4):508-518. PubMed [Evidence: A]
- 8 . Meta-analysis: Enhanced liver fibrosis test to identify hepatic fibrosis in chronic liver diseases, Hinkson A et al. Alimentary Pharmacology & Therapeutics, 2023; 57(7). PubMed [Evidence: A]
- 9 . Elevated liver enzymes and cardiovascular mortality: a systematic review and dose-response meta-analysis of more than one million participants, Rahmani J et al. European Journal of Gastroenterology & Hepatology, 2019; 31(5):555-562. PubMed [Evidence: A]
- 10 . Dietary approaches to stop hypertension (DASH) diet improves hepatic fibrosis, steatosis and liver enzymes in patients with non-alcoholic fatty liver disease: a randomized controlled trial, Sangouni AA et al. European Journal of Nutrition, 2024; 63(2). PubMed [Evidence: B]
Medical Disclaimer
This content is for informational and educational purposes only. It is not intended to provide medical advice or to take the place of such advice or treatment from a personal physician. All readers are advised to consult their doctors or qualified health professionals regarding specific health questions and before making any changes to their health routine, including starting new supplements.
Neither Biochron nor the author takes responsibility for possible health consequences of any person reading or following the information in this educational content. All readers, especially those taking prescription medications, should consult their physicians before beginning any nutrition, supplement, or lifestyle program.
If you have a medical emergency, call your doctor or emergency services immediately.






