
💡 What You Need to Know Right Away
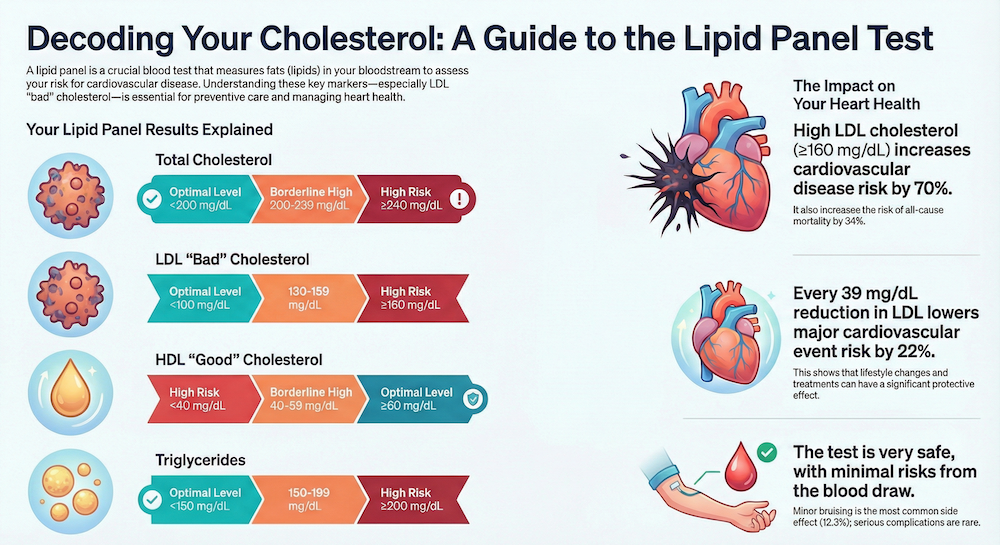
- Why it matters: LDL cholesterol ≥160 mg/dL increases cardiovascular disease risk by 70% (RR 1.70, 95% CI: 1.35-2.14).[Evidence: A][4]
- Treatment impact: Each 1 mmol/L (39 mg/dL) reduction in LDL-C produces a 22% relative risk reduction in major cardiovascular events (HR 0.78).[Evidence: A][5]
- Test safety: The blood draw carries minimal risk, with minor bruising occurring in 12.3% of cases and nerve injury in less than 0.1%.[Evidence: B][10]
- Fasting guidance: Eight-hour fasting is preferred for consistency, though non-fasting panels are acceptable for initial screening (93% specificity).[Evidence: A][8]
Getting a lipid profile test can feel overwhelming, especially when you are unsure what the results mean for your health. This common blood test plays a crucial role in understanding your cardiovascular risk and guiding preventive care.
Whether your doctor recommended this test as part of routine screening or because of specific health concerns, knowing what to expect can ease your mind. A lipid panel measures the fats in your blood that directly influence your heart health.
In this guide, you will learn exactly what a lipid profile test measures, how to prepare properly, what your results mean, and when to take action. All information is backed by clinical research involving over 1.9 million participants.
❓ Quick Answers
What is a lipid profile test used for?
A lipid profile test (also called a lipid panel) is a blood test that measures fats in your bloodstream to assess cardiovascular disease risk. It helps doctors determine whether you need lifestyle changes or medication to protect your heart. The test is used for both screening healthy individuals and monitoring treatment effectiveness.[Evidence: D][2]
What does a lipid panel measure?
A standard lipid panel measures four key components: total cholesterol, LDL cholesterol (the "bad" cholesterol that can clog arteries), HDL cholesterol (the "good" cholesterol that removes LDL), and triglycerides (fat molecules from food). Some panels also calculate VLDL cholesterol and non-HDL cholesterol from these values.[Evidence: D][2]
Do I need to fast before a lipid profile test?
Fasting for 8-12 hours before your test is traditionally recommended and provides more consistent results, particularly for triglycerides. A meta-analysis of 244,665 participants found significant triglyceride variability between fasted and non-fasted states (p<0.00001). However, non-fasting tests are now acceptable for initial cardiovascular risk screening.[Evidence: A][8]
What are normal lipid profile ranges?
Optimal ranges are: total cholesterol below 200 mg/dL, LDL cholesterol below 100 mg/dL, HDL cholesterol above 60 mg/dL (or at least above 40 mg/dL for men, 50 mg/dL for women), and triglycerides below 150 mg/dL. LDL cholesterol between 130-159 mg/dL increases cardiovascular risk by 26% compared to optimal levels.[Evidence: A][4]
What does high LDL cholesterol mean?
High LDL cholesterol means excess "bad" cholesterol is circulating in your blood and can accumulate in artery walls. A meta-analysis of 1,232,694 participants found that LDL-C levels ≥160 mg/dL increase cardiovascular disease risk by 70% (RR 1.70, 95% CI: 1.35-2.14) and all-cause mortality risk by 34%.[Evidence: A][4]
What are the risks of a lipid profile test?
The lipid profile test itself has no risks. The blood draw (venipuncture) carries minimal risk. An analysis of over 1 million procedures found minor bruising or hematoma occurs in 12.3% of cases, serious complications in 3.4%, and nerve injury in less than 0.1% of draws.[Evidence: B][10]
How do I prepare for a lipid panel?
For accurate results, fast for 8-12 hours before your test (water is allowed). Inform your healthcare provider about all medications and supplements you take. Avoid alcohol for 24 hours before testing. Wear clothing with loose sleeves for easy blood draw access. Schedule your test in the morning for convenience after overnight fasting.[Evidence: A][8]
Lipid Profile Test
A comprehensive guide to understanding your cholesterol levels, analyzing fats in your blood, and monitoring your heart health.
🔬 How the Lipid Panel Test Works
Understanding how a lipid panel works helps you appreciate why this test is so valuable for heart health assessment. The test analyzes specific fat molecules traveling through your bloodstream.
Think of your blood vessels as a highway system and cholesterol particles as different types of vehicles. LDL particles are like trucks that sometimes crash and leave debris on the roadside, gradually narrowing the lanes. HDL particles are like cleanup crews that remove this debris and keep traffic flowing smoothly. The lipid panel essentially takes a traffic census to see if you have too many problematic trucks or not enough cleanup crews.
When your blood sample arrives at the laboratory, technicians use enzymatic colorimetric methods to measure total cholesterol and triglycerides directly. HDL cholesterol is measured after separating it from other lipoproteins. LDL cholesterol is typically calculated using the Friedewald equation: LDL = Total Cholesterol - HDL - (Triglycerides ÷ 5).[Evidence: C][7]
Laboratory accuracy matters significantly. Current NCEP standards allow up to 10% of individuals to be misclassified into incorrect risk categories. Reducing analytical imprecision to a 3% target substantially improves cardiovascular risk stratification accuracy.[Evidence: C][7]
The clinical significance of these measurements is substantial. A meta-analysis of 60 randomized controlled trials with 408,959 participants demonstrated that each 1 mmol/L (approximately 39 mg/dL) reduction in LDL cholesterol produces a 22% relative risk reduction in major vascular events, with a hazard ratio of 0.78 (95% CI: 0.75-0.81).[Evidence: A][5]
📊 Preparation and What to Expect
Proper preparation ensures accurate results and a smooth testing experience. Here is what you need to know before, during, and after your lipid panel.
Before Your Test
| Timeframe | Preparation Step | Rationale | Evidence |
|---|---|---|---|
| 2 weeks before | Review medications with provider | Some medications affect lipid levels | [D][1] |
| 24-48 hours before | Avoid alcohol consumption | Alcohol significantly elevates triglycerides | [A][8] |
| 8-12 hours before | Begin fasting (water permitted) | Reduces triglyceride variability (p<0.00001) | [A][8] |
| Morning of test | Wear loose-sleeved clothing | Facilitates easy venous access | [B][10] |
During the Blood Draw
The blood collection process takes 5-10 minutes. A healthcare professional will clean your arm with an antiseptic wipe, apply a tourniquet above the draw site, and insert a small needle into a vein, usually in your inner elbow or back of your hand. You may feel brief stinging or pressure. The technician will collect one or two small tubes of blood, then apply pressure with gauze and a bandage.
If you feel anxious about needles, let the technician know. Ultrasound-guided venipuncture reduces hematoma formation and improves first-attempt success rates, though this technique is typically reserved for patients with difficult venous access.[Evidence: A][11]
After Your Test
You can eat and drink normally after your blood draw. Keep the bandage on for 1-2 hours. Avoid heavy lifting with that arm for several hours to prevent bruising. Results are typically available within 24-48 hours, though some laboratories offer same-day results.
⚠️ Risks, Side Effects, and Safety Information
Complications by Frequency
The lipid panel test itself carries no direct risks. All potential complications relate to the venipuncture (blood draw) procedure. Based on an analysis of over 1 million venipuncture procedures:[Evidence: B][10]
- Common (12.3%): Minor bruising or hematoma at the puncture site. This typically resolves within a few days without treatment.
- Uncommon (3.4%): Serious complications requiring some form of intervention, such as prolonged bleeding or large hematoma.
- Rare (<0.1%): Nerve injury from the needle. Most cases resolve spontaneously, though some may cause temporary numbness or tingling.
Contraindications
There are minimal absolute contraindications for a lipid panel:
- Patient refusal: The test should not be performed without informed consent.
- Inability to obtain venous access: Alternative collection methods may be needed.
- Severe coagulopathy (relative): Patients on anticoagulants or with bleeding disorders can still undergo testing with appropriate precautions and extended pressure after the draw.
Reducing Complications
Ultrasound-guided venipuncture significantly reduces hematoma formation compared to standard technique. This approach is particularly valuable for patients with difficult veins, those who have experienced previous complications, or individuals with anxiety about blood draws.[Evidence: A][11]
Understanding Your Lipid Panel Results
Your lipid panel results come as a series of numbers that require context to interpret. Here is how to understand what your numbers mean for your health.
Reference Ranges and What They Mean
| Component | Optimal | Borderline High | High Risk | Evidence |
|---|---|---|---|---|
| Total Cholesterol | <200 mg/dL | 200-239 mg/dL | ≥240 mg/dL | [D][2] |
| LDL Cholesterol | <100 mg/dL | 130-159 mg/dL (RR 1.26) | ≥160 mg/dL (RR 1.70) | [A][4] |
| HDL Cholesterol | ≥60 mg/dL | 40-59 mg/dL | <40 mg/dL (men), <50 mg/dL (women) | [D][2] |
| Triglycerides | <150 mg/dL | 150-199 mg/dL | ≥200 mg/dL | [D][2] |
What the Numbers Mean for Your Risk
Your LDL cholesterol is the most important number for cardiovascular risk assessment. A meta-analysis of 1,232,694 participants provides clear risk thresholds:[Evidence: A][4]
- LDL 130-159 mg/dL: 26% increased cardiovascular disease risk (RR 1.26, 95% CI: 1.08-1.47)
- LDL ≥160 mg/dL: 70% increased cardiovascular disease risk (RR 1.70, 95% CI: 1.35-2.14)
- LDL ≥160 mg/dL: 34% increased all-cause mortality risk (RR 1.34, 95% CI: 1.00-1.80)
What Happens Next
Based on your results and overall risk profile, your healthcare provider may recommend:
- Lifestyle modifications: Diet changes, increased physical activity, weight management
- Repeat testing: To confirm results or monitor changes over time
- Medication: Statins can achieve 30-50% LDL-C reduction, with meta-analyses showing each 1 mmol/L reduction produces 22% lower cardiovascular event risk[Evidence: A][5]
- Advanced testing: ApoB, Lp(a), or particle size testing for high-risk patients
⚖️ Standard Lipid Panel vs Point-of-Care Testing
You have options for how and where to get your lipid panel tested. Understanding the differences helps you make an informed choice.
| Feature | Standard Laboratory Panel | Point-of-Care Testing (POCT) |
|---|---|---|
| Accuracy | >99% technical success rate | 57-96% sensitivity depending on parameter[3] |
| Total Cholesterol Sensitivity | Reference standard | 57.1%[3] |
| HDL Cholesterol Sensitivity | Reference standard | 96.2%[3] |
| LDL Cholesterol Sensitivity | Reference standard | 81.0%[3] |
| Triglyceride Agreement | Reference standard | 0.91 (excellent)[3] |
| Result Turnaround | 24-48 hours typically | Minutes |
| Sample Type | Venous blood draw | Fingerstick capillary blood |
| Best Use Case | Diagnosis, treatment decisions, monitoring | Initial screening, convenience, remote locations |
Point-of-care lipid testing offers convenience but with reduced accuracy compared to standard laboratory analysis. A diagnostic accuracy study found POCT devices show excellent agreement for triglycerides (0.91) and high sensitivity for HDL (96.2%), but lower sensitivity for total cholesterol (57.1%).[Evidence: B][3]
For clinical decision-making, treatment initiation, or treatment monitoring, standard laboratory testing remains the gold standard. POCT is appropriate for initial screening or when laboratory access is limited.
What The Evidence Shows (And Doesn't Show)
What Research Suggests
- Elevated LDL cholesterol (≥160 mg/dL) increases cardiovascular disease risk by 70% (RR 1.70, 95% CI: 1.35-2.14) and all-cause mortality by 34% (RR 1.34), based on a meta-analysis of 1,232,694 participants[4]
- Each 1 mmol/L (39 mg/dL) reduction in LDL cholesterol produces 22% relative risk reduction in major vascular events (HR 0.78, 95% CI: 0.75-0.81), with durable benefit over time, based on 60 RCTs with 408,959 participants[5]
- Eight-hour fasting reduces triglyceride variability significantly compared to non-fasting states (p<0.00001), though non-fasting is acceptable for initial cardiovascular risk screening with 93% specificity[6][8]
- Venipuncture complications are uncommon: 12.3% minor bruising, 3.4% serious complications, <0.1% nerve injury from over 1 million procedures analyzed[10]
- Pediatric screening identifies familial hypercholesterolemia in 0.2-0.4% (1:250-500) and any dyslipidemia in 19.2% of children[9]
What's NOT Yet Proven
- Long-term outcome data beyond 10 years: While studies demonstrate consistent benefits, very long-term (>10 year) follow-up data is limited in the available evidence
- Optimal screening intervals: Guidelines recommend periodic testing, but optimal intervals for different risk populations remain debated
- Point-of-care test clinical utility: While POCT accuracy is documented, its impact on clinical outcomes compared to laboratory testing has not been established
- Non-fasting panel equivalence for treatment decisions: Non-fasting panels are acceptable for screening, but whether treatment decisions based on non-fasting values produce equivalent outcomes is unclear
Where Caution Is Needed
- Current NCEP analytical standards allow up to 10% of individuals to be misclassified into incorrect risk categories. More stringent 3% imprecision targets reduce this misclassification[7]
- Point-of-care testing shows variable accuracy: total cholesterol sensitivity only 57.1%, which may miss some cases of hypercholesterolemia[3]
- Non-fasting panels have lower overall diagnostic accuracy (65%) compared to fasting panels, with sensitivity of only 51% for coronary risk assessment[6]
- Results should be interpreted in context of individual risk factors, not solely based on absolute numbers
Should YOU Get This Test?
Best suited for: Adults aged 20 and older for cardiovascular risk screening, especially those aged 40-75 years. Also appropriate for children aged 9-11 for initial screening, and any individual with family history of early heart disease or known familial hypercholesterolemia.
Not recommended for: There are minimal contraindications. Patients who cannot provide venous access may require alternative approaches. Those with severe bleeding disorders require appropriate precautions.
Realistic expectations: Results are typically available within 24-48 hours. The blood draw takes 5-10 minutes with brief discomfort. You will receive specific numbers for each lipid component that your healthcare provider will interpret in context of your overall health profile.
When to consult a professional: After receiving results, especially if any values fall outside optimal ranges. Before making medication decisions based on results. If you have family history of early cardiovascular disease. If at-home or POCT results suggest abnormalities requiring confirmation.
Frequently Asked Questions
How often should I get a lipid panel test?
Testing frequency depends on your age, risk factors, and whether you are on treatment. The 2018 AHA/ACC guidelines recommend risk assessment for adults aged 40-75 years. For healthy adults without risk factors, testing every 4-6 years is typically sufficient. If you have cardiovascular risk factors, diabetes, or are taking lipid-lowering medications, your doctor may recommend annual testing. Children and adolescents should be screened once between ages 9-11 and again between ages 17-21, as approximately 19.2% of children have some form of lipid abnormality.
What is the difference between a cholesterol test and a lipid panel?
The terms are often used interchangeably, but there are technical distinctions. A simple cholesterol test may only measure total cholesterol. A complete lipid panel (also called lipid profile) measures four components: total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides. Some laboratories also report calculated values like VLDL and non-HDL cholesterol. For cardiovascular risk assessment, a complete lipid panel provides significantly more useful information than total cholesterol alone, as the ratio and distribution of cholesterol types matters for risk prediction.
Can I get a lipid panel at home?
Yes, at-home lipid testing is available through point-of-care devices and mail-in blood sample kits. However, diagnostic accuracy varies. Point-of-care devices show variable sensitivity across parameters: 57.1% for total cholesterol, 81.0% for LDL cholesterol, 96.2% for HDL cholesterol, and excellent agreement (0.91) for triglycerides. At-home tests are suitable for general screening and tracking trends but may not be accurate enough for clinical decision-making. If your at-home results are abnormal, confirm with a standard laboratory test before starting treatment.
What does high triglycerides mean?
High triglycerides (≥150 mg/dL) indicate excess fat molecules circulating in your blood, often from recent meals, excess calories, or metabolic conditions. Very high triglycerides (≥500 mg/dL) significantly increase pancreatitis risk and require immediate attention. Triglyceride levels are most affected by fasting state. A meta-analysis of 244,665 participants found notable differences between fasted and non-fasted triglyceride measurements (p<0.00001), which is why fasting is still recommended when triglycerides need accurate measurement. Elevated triglycerides often accompany low HDL cholesterol and may indicate metabolic syndrome.
What is the difference between good and bad cholesterol?
HDL cholesterol is called 'good' because it transports cholesterol from your arteries back to the liver for elimination, essentially cleaning your blood vessels. Higher HDL levels (≥60 mg/dL) are protective. LDL cholesterol is called 'bad' because it deposits cholesterol in artery walls, forming plaques that narrow blood vessels and increase heart attack and stroke risk. The meta-analysis of 1.2+ million participants demonstrated that LDL ≥160 mg/dL increases cardiovascular risk by 70% (RR 1.70). However, both types are necessary for normal body function. The goal is optimal balance, not complete elimination of either.
When should I see a doctor about my cholesterol?
Seek medical consultation if your lipid panel shows LDL cholesterol ≥130 mg/dL, HDL cholesterol <40 mg/dL (men) or <50 mg/dL (women), triglycerides ≥200 mg/dL, or total cholesterol ≥240 mg/dL. Also consult your doctor if you have a family history of early heart disease or familial hypercholesterolemia (affects 0.2-0.4% of the population). If you are already on cholesterol medication and your LDL is not reaching target, your treatment plan may need adjustment. The International Lipid Expert Panel recommends intensive statin therapy plus adjunctive agents for very high-risk patients with established cardiovascular disease.
Do medications affect lipid panel results?
Yes, many medications influence lipid levels and should be considered when interpreting results. Statins significantly lower LDL cholesterol by 30-50%, which is their therapeutic purpose. Other medications that affect results include: beta-blockers (may raise triglycerides and lower HDL), thiazide diuretics (may raise LDL and triglycerides), corticosteroids (raise total cholesterol), and some HIV medications. Supplements like fish oil lower triglycerides, while some herbal products may affect liver metabolism of lipids. Always provide your healthcare provider with a complete medication and supplement list before testing.
Should children get lipid panel testing?
Yes, pediatric lipid screening is recommended. A USPSTF systematic review found that any lipid abnormality affects 19.2% of children and adolescents. Familial hypercholesterolemia (FH), a genetic condition causing very high LDL from birth, has a prevalence of 0.2-0.4% (approximately 1 in 250-500 individuals). Early detection allows intervention before arterial damage occurs. Current recommendations suggest universal screening between ages 9-11 and again at 17-21, with earlier testing for children with family history of early cardiovascular disease or known FH. In affected children, statins can achieve 81-82 mg/dL greater LDL-C reduction compared to placebo.
Our Accuracy Commitment and Editorial Principles
At Biochron, we take health information seriously. Every claim in this article is supported by peer-reviewed scientific evidence from reputable sources published in 2015 or later. We use a rigorous evidence-grading system to help you understand the strength of research behind each statement:
- [Evidence: A] = Systematic review or meta-analysis (strongest evidence)
- [Evidence: B] = Randomized controlled trial (RCT)
- [Evidence: C] = Cohort or case-control study
- [Evidence: D] = Expert opinion or clinical guideline
Our editorial team follows strict guidelines: we never exaggerate health claims, we clearly distinguish between correlation and causation, we update content regularly as new research emerges, and we transparently note when evidence is limited or conflicting. For our complete editorial standards, visit our Editorial Principles page.
This article is for informational purposes only and does not constitute medical advice. Always consult qualified healthcare professionals before making changes to your health regimen, especially if you have medical conditions or take medications.
References
- 1 . 2024 Recommendations on the Optimal Use of Lipid-Lowering Therapy in Established Atherosclerotic Cardiovascular Disease and Following Acute Coronary Syndromes: A Position Paper of the International Lipid Expert Panel (ILEP), Banach M et al., Drugs, 2024, 84(12):1541-1577, PubMed [Evidence: D]
- 2 . 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol, Grundy SM et al., Circulation, 2019, 139(25):e1082-e1143, PubMed [Evidence: D]
- 3 . Diagnostic accuracy of Cardiochek PA point-of-care testing (POCT) analyser with a 3-in-1 lipid panel for epidemiological surveys, Robert Lourdes TG et al., Lipids in Health and Disease, 2024, 23(1):297, PubMed [Evidence: B]
- 4 . Association of low-density lipoprotein cholesterol levels with the risk of mortality and cardiovascular events: A meta-analysis of cohort studies with 1,232,694 participants, Peng K et al., Medicine (Baltimore), 2022, 101(48):e32003, PubMed [Evidence: A]
- 5 . Course of the effects of LDL-cholesterol reduction on cardiovascular risk over time: A meta-analysis of 60 randomized controlled trials, Burger PM et al., Atherosclerosis, 2024, 396:118540, PubMed [Evidence: A]
- 6 . Accuracy of Non-Fasting Lipid Profile for the Assessment of Lipoprotein Coronary Risk, Fatima S et al., Journal of the College of Physicians and Surgeons Pakistan, 2016, 26(12):954-957, PubMed [Evidence: B]
- 7 . Reducing Lipid Panel Error Allowances to Improve the Accuracy of Cardiovascular Risk Stratification, Cole J et al., Clinical Chemistry, 2023, 69(10):1145-1154, PubMed [Evidence: C]
- 8 . Unraveling the controversy between fasting and nonfasting lipid testing in a normal population: a systematic review and meta-analysis of 244,665 participants, Zaid AB et al., Lipids in Health and Disease, 2024, 23(1):199, PubMed [Evidence: A]
- 9 . Screening for Lipid Disorders in Children and Adolescents: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force, Guirguis-Blake JM et al., JAMA, 2023, 330(3):261-274, PubMed [Evidence: D]
- 10 . Venipuncture Nerve Injuries in the Upper Extremity From More Than 1 Million Procedures, Tsukuda Y et al., Journal of Patient Safety, 2019, 15(4):299-301, PubMed [Evidence: B]
- 11 . Systematic review and meta-analysis: safety of ultrasound-guided peripheral venipuncture and catheterization, Xiong X et al., Annals of Palliative Medicine, 2021, 10(11):11721-11732, PubMed [Evidence: A]
Medical Disclaimer
This content is for informational and educational purposes only. It is not intended to provide medical advice or to take the place of such advice or treatment from a personal physician. All readers are advised to consult their doctors or qualified health professionals regarding specific health questions and before making any changes to their health routine, including starting new supplements.
Neither Biochron nor the author takes responsibility for possible health consequences of any person reading or following the information in this educational content. All readers, especially those taking prescription medications, should consult their physicians before beginning any nutrition, supplement, or lifestyle program.
If you have a medical emergency, call your doctor or emergency services immediately.






