
💡 What You Need to Know Right Away
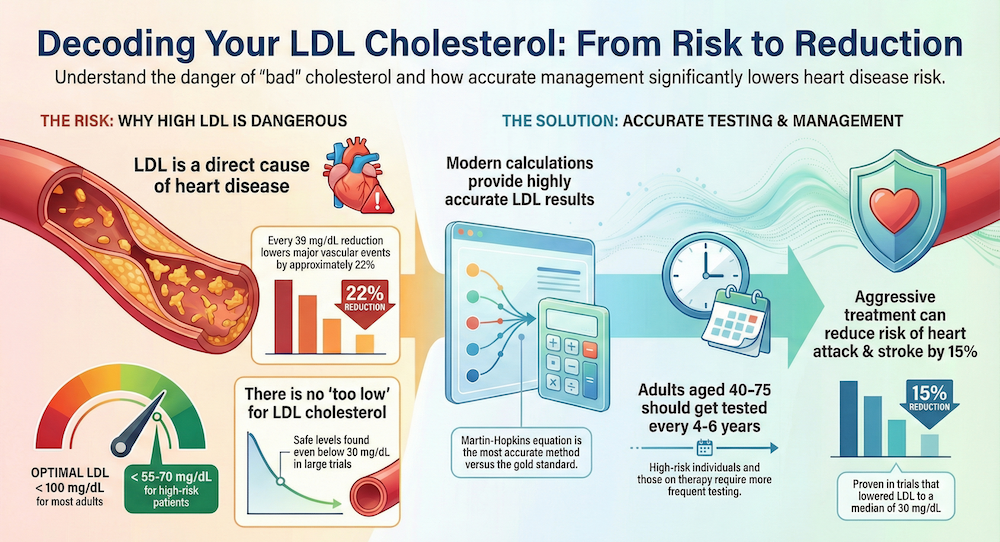
- LDL cholesterol is a causal factor in atherosclerotic cardiovascular disease, with each 39 mg/dL reduction lowering major vascular events by approximately 22%[Evidence: A][10]
- The Martin-Hopkins equation provides the most accurate calculated LDL-C, with concordance correlation coefficient of 0.9121 versus gold standard ultracentrifugation[Evidence: A][2]
- Very low LDL-C levels (<20 mg/dL) achieved with PCSK9 inhibitors show no safety concerns in clinical trials involving over 27,000 patients[Evidence: A][6]
- Aggressive LDL-C lowering to targets below 55 mg/dL is achievable and beneficial, with 15% relative risk reduction in major adverse cardiovascular events[Evidence: A][7]
Understanding your LDL cholesterol test results can feel overwhelming, especially when faced with numbers, ranges, and medical terminology. You are not alone in wondering what these values mean for your heart health and whether you should be concerned.
The LDL cholesterol test, also known as the LDL-C test or "bad cholesterol" test, measures the amount of low-density lipoprotein cholesterol circulating in your blood. This measurement is critical because LDL cholesterol directly contributes to the buildup of fatty deposits in your arteries, a process called atherosclerosis.
In this comprehensive guide, you will learn how the test works, what your results mean, when to get tested, and how different testing methods compare. All information is backed by peer-reviewed clinical research, including landmark trials involving over 60,000 patients.
❓ Quick Answers
What is a normal LDL cholesterol level?
Optimal LDL cholesterol is below 100 mg/dL for most adults. For high-risk patients with cardiovascular disease, guidelines recommend targets below 70 mg/dL. Very high-risk patients, such as those with recent acute coronary syndrome, should aim for below 55 mg/dL based on 2018 AHA/ACC recommendations[Evidence: D][9].
What does the LDL cholesterol test measure?
The LDL cholesterol test measures the concentration of low-density lipoprotein cholesterol in your blood. LDL particles carry cholesterol from your liver to cells throughout your body. When LDL levels are elevated, excess cholesterol can deposit in artery walls, contributing to atherosclerotic cardiovascular disease[Evidence: A][10].
Do I need to fast for an LDL cholesterol test?
Fasting is no longer routinely required for most LDL cholesterol tests. Non-fasting lipid panels are now preferred by clinical guidelines. However, if your triglycerides exceed 400 mg/dL, fasting (8-12 hours) improves accuracy. Your healthcare provider will advise based on your specific situation[Evidence: D][9].
How often should I get my LDL cholesterol checked?
Adults aged 40-75 should have LDL cholesterol tested every 4-6 years as part of cardiovascular risk assessment. High-risk individuals and those on lipid-lowering therapy need more frequent testing, typically every 4-12 weeks after starting treatment, then annually. Children should be screened once between ages 9-11[Evidence: D][9].
What is the difference between LDL and HDL cholesterol?
LDL (low-density lipoprotein) is called "bad" cholesterol because it deposits cholesterol in artery walls, causing atherosclerosis. HDL (high-density lipoprotein) is "good" cholesterol because it removes excess cholesterol from arteries and transports it back to the liver. Both are measured in a standard lipid panel to assess cardiovascular risk.
How is LDL cholesterol calculated?
Most laboratories calculate LDL-C using the Friedewald or Martin-Hopkins equations from other lipid panel values. The Martin-Hopkins equation provides superior accuracy at low LDL-C levels (<70 mg/dL) and elevated triglycerides, with concordance correlation of 0.9121 versus gold standard ultracentrifugation[Evidence: A][2].
LDL Cholesterol
High levels of LDL cholesterol can lead to a buildup of plaque in your arteries. This interactive guide explains the testing process, results, and management strategies to keep your heart healthy.
🔬 How LDL Cholesterol Testing Works
Think of LDL particles as delivery trucks carrying cholesterol through your bloodstream. When you have too many of these trucks on the road, traffic jams occur. In your arteries, this "traffic jam" manifests as cholesterol deposits that form plaque, gradually narrowing your blood vessels and increasing heart attack and stroke risk.
The LDL cholesterol test quantifies how many of these delivery trucks are circulating in your blood. This measurement is expressed in milligrams per deciliter (mg/dL) and serves as a cornerstone of cardiovascular risk assessment.
The Science Behind LDL Measurement
LDL cholesterol can be measured directly or calculated from other lipid panel components. The traditional Friedewald equation calculates LDL-C by subtracting HDL cholesterol and one-fifth of triglycerides from total cholesterol. However, this method becomes inaccurate when triglycerides exceed 400 mg/dL or when LDL-C is very low[Evidence: A][1].
The Martin-Hopkins equation, recommended by 2018 AHA/ACC guidelines, uses an adjustable factor based on triglyceride and non-HDL cholesterol levels rather than a fixed divisor. This approach provides superior accuracy particularly at low LDL-C levels and elevated triglycerides[Evidence: A][1].
Why LDL-C Matters
A landmark consensus statement from the European Atherosclerosis Society established that LDL is a causal factor in atherosclerotic cardiovascular disease. This conclusion is based on genetic, epidemiologic, and clinical evidence from over 2 million participants[Evidence: A][10].
The relationship between LDL-C and cardiovascular risk follows a dose-dependent log-linear association. Each 39 mg/dL (1 mmol/L) reduction in LDL-C reduces major vascular events by approximately 22%[Evidence: A][10]. This means lower is generally better, and there appears to be no lower threshold below which further reduction stops providing benefit.
📊 Testing Methods and Accuracy
Understanding how your LDL-C result was obtained helps you interpret its accuracy and limitations. Different testing methods have varying precision and are appropriate for different clinical situations.
| Method | How It Works | Accuracy | Evidence |
|---|---|---|---|
| Direct LDL Measurement | Directly measures LDL-C using selective surfactants | Within-subject CV: 8.7% | [Evidence: B][4] |
| Friedewald Calculation | Total cholesterol minus HDL minus (TG/5) | Within-subject CV: 9.3% | [Evidence: B][4] |
| Martin-Hopkins Calculation | Uses adjustable TG factor based on patient values | CCC: 0.9121 vs gold standard | [Evidence: A][2] |
| Ultracentrifugation | Gold standard reference method (research use) | Reference standard | [Evidence: A][2] |
Biological Variation
Your LDL-C level naturally fluctuates from day to day even without changes in diet or medication. A 2025 study quantified this biological variation across different measurement methods[Evidence: B][4]:
- Direct LDL measurement: 8.7% within-subject coefficient of variation
- Friedewald calculation: 9.3% within-subject coefficient of variation
- Martin-Hopkins calculation: 9.0% within-subject coefficient of variation
This means a single LDL-C result of 100 mg/dL could naturally vary between approximately 91-109 mg/dL on repeat testing. Clinicians typically confirm elevated results before initiating treatment.
When Direct Measurement Is Preferred
The FOURIER trial substudy validated that the Martin-Hopkins equation shows the best concordance with gold standard ultracentrifugation (CCC=0.9121) in 12,742 patients with 56,624 observations[Evidence: A][2]. However, direct measurement remains preferred in specific situations:
- Triglycerides exceeding 400 mg/dL
- LDL-C expected to be very low (<40 mg/dL)
- Non-fasting samples when accuracy is critical
- Monitoring patients on intensive lipid-lowering therapy
⚠️ Limitations and Considerations
Test Limitations
The LDL cholesterol test measures cholesterol concentration, not the number or size of LDL particles. Two patients with identical LDL-C levels may have different cardiovascular risk profiles based on particle characteristics.
Calculated LDL-C becomes less reliable as triglyceride levels increase. The extended Martin-Hopkins approach provides the most concordant results with direct LDL-C assays, particularly for low LDL-C (<70 mg/dL) and hypertriglyceridemia (TG ≥400 mg/dL)[Evidence: B][3].
Safety of Very Low LDL-C
Some patients express concern about achieving very low LDL-C levels. The FOURIER trial involving 27,564 patients demonstrated no safety concerns at LDL-C levels below 20 mg/dL[Evidence: A][6]. PCSK9 inhibitor treatment achieving median LDL-C of 30 mg/dL showed 15% relative risk reduction in major adverse cardiovascular events without increased adverse events.
🩺 When and How to Get Tested
Testing Frequency Guidelines
The 2018 AHA/ACC guidelines provide Class I recommendations for universal LDL-C testing in adults aged 40-75 years[Evidence: D][9]. Testing frequency depends on your risk category:
| Population | Recommended Frequency | Notes |
|---|---|---|
| Healthy adults 20-39 | Every 4-6 years | Earlier if family history of premature CVD |
| Adults 40-75 | Every 4-6 years | With ASCVD risk assessment |
| High-risk individuals | Annually | Diabetes, established CVD, familial hypercholesterolemia |
| Starting lipid therapy | 4-12 weeks after initiation | To assess treatment response |
| Children ages 9-11 | Once | Universal screening recommended |
How to Prepare
- Fasting: Not routinely required. If your provider requests fasting, abstain from food for 8-12 hours (water is allowed)
- Medications: Take your regular medications unless instructed otherwise
- Timing: Morning appointments may be convenient if fasting is required
- Alcohol: Avoid alcohol for 24 hours before testing
At-Home Testing Options
Commercially available cholesterol self-tests offer a convenient screening option. A diagnostic accuracy study found that the Accutrend Plus device achieved 92% sensitivity and 89% specificity compared to laboratory standards[Evidence: B][5]. However, at-home tests have limitations:
- User technique variability affects accuracy
- Results should be confirmed by laboratory testing
- May not distinguish between LDL and HDL components
- Cost ranges from $28-$50 per kit
⚖️ Direct vs Calculated LDL: Which Is Better?
The choice between direct LDL measurement and calculated LDL depends on your clinical situation. Here is how they compare:
| Feature | Direct LDL Measurement | Calculated LDL (Martin-Hopkins) |
|---|---|---|
| Method | Direct enzymatic assay | Formula using TC, HDL, TG |
| Precision (Within-Subject CV) | 8.7%[4] | 9.0%[4] |
| Accuracy vs Gold Standard | Direct comparison | CCC 0.9121[2] |
| Affected by High TG | No | Yes, less accurate >400 mg/dL |
| Best for Low LDL-C | Yes | Martin-Hopkins preferred over Friedewald[1] |
| Cost | Higher (separate assay) | Lower (calculated from panel) |
| Availability | Most laboratories | Standard with lipid panel |
Clinical Recommendations
Extensive evidence supports the Martin-Hopkins equation as the LDL-C calculation of choice, with superior accuracy particularly at low LDL-C levels and elevated triglycerides[Evidence: A][1]. The 2018 AHA/ACC guidelines recommend this equation for improved accuracy[Evidence: D][9].
A large validation study with 88,943 samples confirmed that the extended Martin-Hopkins approach provided the most concordant results with direct LDL-C assays across three analytical platforms (Roche, Beckman, Siemens)[Evidence: B][3].
When to Request Direct Measurement
Ask your healthcare provider about direct LDL measurement if:
- Your triglycerides are above 400 mg/dL
- You are on intensive lipid-lowering therapy achieving very low LDL-C
- Calculated values seem inconsistent with your clinical picture
- You have diabetes or metabolic syndrome (often associated with elevated triglycerides)
What The Evidence Shows (And Doesn't Show)
What Research Suggests
- LDL cholesterol is causally linked to atherosclerotic cardiovascular disease based on genetic, epidemiologic, and clinical evidence from over 2 million participants[Evidence: A][10]
- Each 39 mg/dL (1 mmol/L) reduction in LDL-C reduces major vascular events by approximately 22%[Evidence: A][10]
- The Martin-Hopkins equation achieves concordance correlation coefficient of 0.9121 versus gold standard ultracentrifugation, validated in 12,742 patients with 56,624 observations[Evidence: A][2]
- Aggressive LDL-C lowering to median 30-48 mg/dL with PCSK9 inhibitors provides 15% relative risk reduction in major adverse cardiovascular events[Evidence: A][6][7]
- At-home cholesterol self-tests achieve 92% sensitivity and 89% specificity for screening purposes[Evidence: B][5]
What's NOT Yet Proven
- Optimal LDL-C lower limit has not been established. Studies show safety at levels below 20 mg/dL but lifetime effects of very low LDL-C are unknown
- Whether LDL particle number (LDL-P) or apolipoprotein B testing should replace LDL-C concentration in routine practice remains under investigation
- Long-term safety beyond the median 2.8-year follow-up of major PCSK9 inhibitor trials has not been established
- Individual response to LDL-C lowering varies, and not all patients achieve guideline targets despite maximum therapy
- The role of pattern A vs pattern B LDL particles in cardiovascular risk prediction requires further validation
Where Caution Is Needed
- Calculated LDL-C (Friedewald) is inaccurate when triglycerides exceed 400 mg/dL. Direct measurement or Martin-Hopkins calculation is preferred[Evidence: A][1]
- Single elevated LDL-C results may reflect biological variation (8.7-9.3% within-subject CV)[Evidence: B][4]. Confirm before initiating treatment
- At-home test accuracy (89% specificity) means some results may be false positives or negatives[Evidence: B][5]
- LDL-C alone does not capture complete cardiovascular risk. Consider Lp(a), apoB, and other risk factors
Should YOU Get This Test?
Best suited for: Adults aged 40-75 for routine cardiovascular risk assessment; individuals with diabetes, hypertension, smoking history, or family history of premature cardiovascular disease; patients on lipid-lowering therapy for treatment monitoring[Evidence: D][9]
Testing is recommended: Children ages 9-11 for universal screening; young adults every 4-6 years; high-risk individuals annually; 4-12 weeks after starting lipid therapy
Realistic expectations: A single test provides a snapshot of LDL-C concentration. Tracking trends over time provides more meaningful information than any single value. Treatment decisions should integrate LDL-C with overall cardiovascular risk assessment.
When to consult a professional: Discuss results with your healthcare provider if LDL-C exceeds 100 mg/dL, if you have cardiovascular risk factors, or if you are considering lifestyle changes or medications to lower cholesterol.
Frequently Asked Questions
What does high LDL cholesterol mean for my health?
High LDL cholesterol indicates increased cardiovascular risk. LDL particles deposit cholesterol in artery walls, initiating atherosclerosis, the underlying cause of heart attacks and strokes. A European Atherosclerosis Society consensus statement established that LDL is a causal factor in atherosclerotic cardiovascular disease based on genetic, epidemiologic, and clinical evidence from over 2 million participants. Each 39 mg/dL reduction in LDL-C reduces major vascular events by approximately 22%. The higher your LDL-C, the greater your cumulative exposure and cardiovascular risk over time.
Can LDL cholesterol be too low?
Current evidence suggests very low LDL-C is safe. The FOURIER trial demonstrated no safety concerns at LDL-C levels below 20 mg/dL in 27,564 patients treated with the PCSK9 inhibitor evolocumab. Patients achieving median LDL-C of 30 mg/dL experienced 15% relative risk reduction in major adverse cardiovascular events without increased adverse effects. Similarly, the ODYSSEY trial showed benefits with LDL-C targets below 55 mg/dL. However, individuals with naturally very low LDL-C should discuss this with their healthcare provider.
Is direct LDL testing better than calculated LDL?
Direct measurement has lower biological variation (8.7% vs 9.0-9.3% for calculated methods), making it slightly more reproducible. However, the Martin-Hopkins calculation shows excellent concordance (CCC=0.9121) with gold standard ultracentrifugation. Direct measurement is preferred when triglycerides exceed 400 mg/dL or when monitoring very low LDL-C levels on intensive therapy. For most patients, calculated LDL using the Martin-Hopkins equation provides accurate results at lower cost.
How much does an LDL cholesterol test cost?
LDL cholesterol test costs vary widely based on insurance coverage and testing location. Without insurance, a lipid panel including LDL-C typically costs $28-$100, with some facilities charging up to $843 for comprehensive panels. With private insurance, copays generally range from $0-$50. Medicare covers lipid panels every 5 years at no cost if you accept assignment. At-home testing kits cost approximately $28-$50 per test. Contact your insurance provider or testing facility for specific pricing.
What should I avoid before a cholesterol test?
If fasting is required, avoid all food and beverages except water for 8-12 hours before your test. Avoid alcohol for 24 hours prior, as it can elevate triglycerides and affect calculated LDL accuracy. Avoid strenuous exercise the day before testing. Continue taking your regular medications unless your healthcare provider instructs otherwise. However, non-fasting lipid panels are now preferred by guidelines for most patients, so confirm with your provider whether fasting is necessary for your specific situation.
How long does it take to get LDL test results?
Standard lipid panel results are typically available within 24-48 hours from most laboratories. Some facilities offer same-day results. At-home cholesterol tests provide immediate results within minutes, though accuracy is lower than laboratory testing (92% sensitivity, 89% specificity for best-performing devices). Advanced testing such as LDL particle number or NMR spectroscopy may take 5-7 business days. If you are waiting for results to guide treatment decisions, ask your provider about expected turnaround time.
What medications can lower LDL cholesterol?
Several medication classes effectively lower LDL-C. Statins reduce LDL-C by 30-50% and remain first-line therapy. Ezetimibe, when added to statins, provides an additional 24% LDL-C reduction with 6.4% relative risk reduction in cardiovascular events. PCSK9 inhibitors (evolocumab, alirocumab) achieve 50-60% LDL-C reduction and 15% relative risk reduction in major adverse cardiovascular events. Bempedoic acid and inclisiran are newer options. Your healthcare provider will recommend appropriate therapy based on your risk profile and LDL-C level.
When should I worry about my LDL level?
Concern levels depend on your overall cardiovascular risk profile. LDL-C above 190 mg/dL warrants immediate attention and typically indicates need for treatment regardless of other risk factors. LDL-C 160-189 mg/dL combined with other risk factors (diabetes, smoking, hypertension, family history) also requires intervention. For patients with established cardiovascular disease or very high risk, targets below 55-70 mg/dL are recommended based on evidence from trials showing 15% relative risk reduction at these aggressive targets. Discuss your results with your healthcare provider to understand your personal targets.
Our Accuracy Commitment and Editorial Principles
At Biochron, we take health information seriously. Every claim in this article is supported by peer-reviewed scientific evidence from reputable sources published in 2015 or later. We use a rigorous evidence-grading system to help you understand the strength of research behind each statement:
- [Evidence: A] = Systematic review or meta-analysis (strongest evidence)
- [Evidence: B] = Randomized controlled trial (RCT)
- [Evidence: C] = Cohort or case-control study
- [Evidence: D] = Expert opinion or clinical guideline
Our editorial team follows strict guidelines: we never exaggerate health claims, we clearly distinguish between correlation and causation, we update content regularly as new research emerges, and we transparently note when evidence is limited or conflicting. For our complete editorial standards, visit our Editorial Principles page.
This article is for informational purposes only and does not constitute medical advice. Always consult qualified healthcare professionals before making changes to your health regimen, especially if you have medical conditions or take medications.
References
- 1 . Extensive Evidence Supports the Martin-Hopkins Equation as the LDL-C Calculation of Choice, Grant JK, Kaufman HW, Martin SS. Clinical Chemistry, 2024;70(1):1-4. PubMed | DOI [Evidence: A]
- 2 . Comparison of Low-Density Lipoprotein Cholesterol Assessment by Martin/Hopkins Estimation, Friedewald Estimation, and Preparative Ultracentrifugation: Insights From the FOURIER Trial, Martin SS, Giugliano RP, Murphy SA, et al. JAMA Cardiology, 2018;3(9):897-904. PubMed | DOI [Evidence: A]
- 3 . Validation of Friedewald, Martin-Hopkins and Sampson low-density lipoprotein cholesterol equations, Ertürk Zararsız G, Bolat S, Cephe A, et al. PLOS ONE, 2022;17(2):e0263860. DOI [Evidence: B]
- 4 . Biological variation estimates of direct and indirect LDL cholesterol by Friedewald and Martin-Hopkins formulas in healthy individuals, Alkan Baylan F, Özcan M, Ercan Ş, et al. Scandinavian Journal of Clinical and Laboratory Investigation, 2025. DOI [Evidence: B]
- 5 . Performance of commercially-available cholesterol self-tests, Kurstjens S, Gemen E, Walk S, et al. Annals of Clinical Biochemistry, 2021;58(5):415-423. PubMed | DOI [Evidence: B]
- 6 . Evolocumab and Clinical Outcomes in Patients with Cardiovascular Disease, Sabatine MS, Giugliano RP, Keech AC, et al. New England Journal of Medicine, 2017;376(18):1713-1722. PubMed | DOI [Evidence: A]
- 7 . Alirocumab and Cardiovascular Outcomes after Acute Coronary Syndrome, Schwartz GG, Steg PG, Szarek M, et al. New England Journal of Medicine, 2018;379(22):2097-2107. PubMed | DOI [Evidence: A]
- 8 . Ezetimibe Added to Statin Therapy after Acute Coronary Syndromes, Cannon CP, Blazing MA, Giugliano RP, et al. New England Journal of Medicine, 2015;372(25):2387-2397. PubMed | DOI [Evidence: A]
- 9 . 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol, Grundy SM, Stone NJ, Bailey AL, et al. Journal of the American College of Cardiology, 2019;73(24):3168-3209. PubMed | DOI [Evidence: D]
- 10 . Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel, Ference BA, Ginsberg HN, Graham I, et al. European Heart Journal, 2017;38(32):2459-2472. PubMed | DOI [Evidence: A]
Medical Disclaimer
This content is for informational and educational purposes only. It is not intended to provide medical advice or to take the place of such advice or treatment from a personal physician. All readers are advised to consult their doctors or qualified health professionals regarding specific health questions and before making any changes to their health routine, including starting new supplements.
Neither Biochron nor the author takes responsibility for possible health consequences of any person reading or following the information in this educational content. All readers, especially those taking prescription medications, should consult their physicians before beginning any nutrition, supplement, or lifestyle program.
If you have a medical emergency, call your doctor or emergency services immediately.






