
💡 What You Need to Know Right Away
A knee MRI is an imaging test that uses magnetic fields and radio waves to create detailed pictures of your knee's bones, cartilage, ligaments, and tendons, helping doctors diagnose injuries, arthritis, and unexplained pain without radiation or needles.
Also known as: MRI of the knee, knee MR imaging, knee magnetic resonance imaging, MRI knee scan
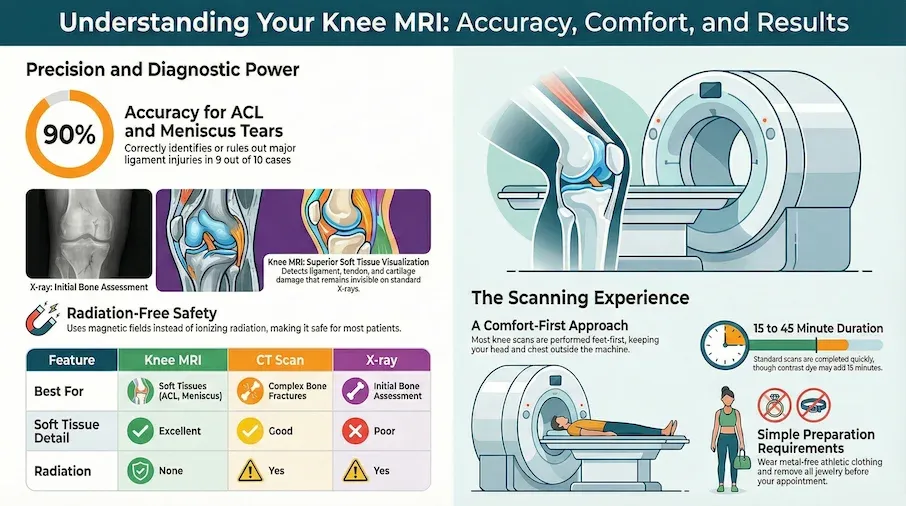
- Research shows knee MRI correctly identifies ACL tears in about 9 out of 10 cases and rules them out in over 9 out of 10 cases[Evidence: A][1]
- Research shows knee MRI correctly identifies medial meniscus tears in 9 out of 10 cases[Evidence: A][4]
- The scan takes 15-45 minutes without contrast dye, or 30-60 minutes with contrast[Evidence: D][3]
- Fear of enclosed spaces causes fewer than 2 out of 100 scans to be incomplete[Evidence: C][12]
If your doctor has recommended a knee MRI, you may be wondering what to expect and whether the procedure will be uncomfortable. It's common to feel anxious about medical tests, especially ones that involve lying still in a narrow machine.
The good news is that knee MRI is one of the easier scans to undergo. Unlike brain or spine MRIs where your whole body enters the machine, for a knee scan only your lower body goes inside the tunnel. Your chest and head typically remain outside, which most people find much more comfortable.
In this guide, you'll learn exactly what happens during a knee MRI, how accurate the test is at detecting injuries, what to do if you're claustrophobic, and how to prepare for your appointment. Whether you're dealing with sports injuries, unexplained knee pain, or need imaging before surgery, this information will help you feel confident and prepared.
❓ Quick Answers
What does a knee MRI show?
A knee MRI shows detailed images of bones, cartilage, tendons, ligaments, muscles, and blood vessels inside your knee joint. It can detect meniscus tears, ACL and PCL injuries, cartilage damage, bone fractures not visible on X-ray, cysts, tumors, and infections. Research shows knee MRI correctly identifies meniscus tears in about 9 out of 10 cases[Evidence: A][1].
How long does a knee MRI take?
A standard knee MRI takes 15-45 minutes without contrast dye. If contrast dye is used, expect 30-60 minutes. Your total appointment time will be 45-65 minutes including check-in, changing clothes, and positioning[Evidence: D][3]. Most people spend 20-30 minutes inside the scanner.
Is a knee MRI painful?
Knee MRI is painless. The scan uses magnetic fields and radio waves, not needles or radiation. You may feel uncomfortable lying still for 20-45 minutes, and the machine makes loud knocking sounds, but there is no pain. If contrast is used, you'll feel a brief needle stick similar to a blood draw[Evidence: D][3].
Do you need contrast dye for a knee MRI?
Most routine knee MRIs do not require contrast dye. Contrast may be used when doctors need to evaluate inflammation, tumors, infections, or blood vessel problems. Research shows gadolinium-based contrast agents are safe and well tolerated, with acute adverse reactions being rare[Evidence: A][5].
Can I have a knee MRI if I'm claustrophobic?
Yes. Knee MRI is easier for claustrophobic patients because only your lower body enters the scanner. Your chest and head remain outside the tunnel. Early research suggests fear of enclosed spaces causes about 1-2 out of 100 scans to be incomplete[Evidence: C][11]. Options include open MRI machines, sedation, and relaxation techniques.
Can you eat before a knee MRI?
Yes, you can usually eat and drink normally before a knee MRI without contrast. If contrast dye will be used, your facility may ask you to avoid food for 2-4 hours beforehand. If sedation is planned, fasting is required. Follow your specific facility's instructions.
What should I wear to a knee MRI?
Wear comfortable, loose clothing without metal zippers, buttons, or snaps. Athletic wear or sweatpants work well. You'll need to remove jewelry, watches, hearing aids, and any metal objects. Many facilities provide a gown to change into for the scan.
Is knee MRI safe during pregnancy?
MRI does not use radiation and is generally considered safe during pregnancy when medically necessary. Studies suggest no increased risk to the fetus from MRI exposure[Evidence: B][7]. However, gadolinium contrast is typically avoided during pregnancy. Always inform your doctor if you are or might be pregnant.
Knee MRI
A comprehensive guide to understanding how MRI technology visualizes the complex structures of the knee, aiding in the diagnosis of injuries and conditions without radiation.
🔬 How Does a Knee MRI Work?
Think of an MRI scanner as a powerful camera that uses magnets instead of light to photograph the inside of your body. Unlike X-rays that pass radiation through you, MRI uses a strong magnetic field and radio waves to create incredibly detailed images of soft tissues that other imaging cannot see well.
Your body is made mostly of water, and water contains hydrogen atoms. When you enter the MRI machine, the powerful magnet causes the hydrogen atoms in your knee to align in a specific direction. Then, pulses of radio waves are sent through your knee, causing these atoms to spin. When the radio waves stop, the atoms release energy as they return to their original position. Sensors detect this energy and a computer converts it into detailed pictures.
Clinical guidelines recommend using three different viewing angles to capture complete images of the knee[Evidence: D][3]. Specific imaging techniques called T1-weighted and T2-weighted sequences help doctors see different types of tissue clearly. T1-weighted images show fat and bone marrow, while T2-weighted images highlight fluid and swelling, making them excellent for detecting tears and inflammation[Evidence: D][3].
Imagine your knee as a complex machine with many moving parts. The MRI acts like a detailed blueprint, showing the ACL and PCL ligaments that stabilize your knee, the meniscus cartilage that cushions the joint, the tendons that connect muscles to bones, and even the fluid surrounding the joint. This comprehensive review provides doctors with information they cannot get from any other imaging test[Evidence: C][10].
Studies suggest knee MRI provides better detail of soft tissues compared to CT scans[Evidence: B][2]. This makes MRI the preferred choice when doctors need to evaluate ligament tears, cartilage damage, or inflammation that would be invisible on X-rays.
🧪 What to Expect: The Real User Experience
During the Procedure
During the knee MRI, you'll lie on a narrow table that slides into a cylindrical tunnel about 23-26 inches wide, depending on the machine model. For a knee scan, you are positioned feet-first, which means only your lower body enters the machine. Your chest and head remain outside the bore, which most patients find significantly less confining than full-body scans.
The room is kept cool at 65-68°F to maintain equipment performance, and many patients feel cold in the standard hospital gown. The table surface is hard plastic, which may feel cold initially. Foam supports are placed around your knee to keep it completely still. The positioning may feel snug but should not be painful. The technologist will adjust your leg until your knee is centered in the imaging coil.
The machine makes loud banging, knocking, and whirring sounds throughout the scan. These noises can reach 85-100 decibels, similar to a loud concert or lawn mower. You must remain completely motionless during each imaging sequence, which lasts 2-5 minutes. A complete scan involves 6-12 sequences.
What You'll Feel After
After the scan, you can resume normal activities immediately. No recovery time is needed unless you received sedation. Common post-procedure experiences include:
- Minor stiffness or muscle tension from lying still, which resolves within hours
- Mild ear ringing from the machine noise, which typically fades within 1-2 hours
- If contrast was used: a metallic taste lasting 15-30 minutes and mild bruising at the IV site
- If sedation was used: drowsiness for 2-4 hours, requiring a ride home
How to Make It Easier
- For the noise: Request earplugs or headphones with music before the scan starts
- If you're claustrophobic: Ask about open MRI availability at your facility, or request feet-first positioning (standard for knee scans)
- To stay calm: Practice slow, deep breathing (4 counts in, 4 counts out) during the scan
- Before entering: Close your eyes to reduce visual awareness of the confined space
- For safety: You'll receive a squeeze ball that signals the technologist to stop the scan if needed
- For comfort: Empty your bladder before the scan and ask for a blanket if the room feels cold
- For anxiety: Some facilities offer prism glasses that let you see outside the machine while lying down
📊 Procedure Duration and What Happens
Understanding the timeline of your knee MRI appointment helps you plan your day and reduces anxiety about the unknown.
| Step | Duration | What Happens | Evidence |
|---|---|---|---|
| Check-in and paperwork | 5-10 minutes | Verify insurance, sign consent, review safety questionnaire about metal implants | — |
| Change clothes | 5 minutes | Remove metal objects, put on gown if needed | — |
| Positioning | 5-10 minutes | Technologist positions knee in imaging coil, places foam supports, provides earplugs | — |
| Scan without contrast | 15-45 minutes | 6-12 imaging sequences, must remain still | [D][3] |
| IV contrast (if needed) | 10-15 minutes | IV placement, contrast injection, additional sequences | [A][5] |
| Get dressed and depart | 5 minutes | Change back into clothes, collect belongings | — |
Total appointment time: 45-65 minutes for standard knee MRI. Plan for up to 90 minutes if contrast is used or if the facility is busy.
Clinical guidelines emphasize using three orthogonal imaging planes and both T2-weighted fluid-sensitive and T1-weighted sequences to capture comprehensive images of all knee structures[Evidence: D][3].
⚠️ Safety, Risks, and Contraindications
The test itself is painless and uses no radiation, making it one of the safest imaging methods available. Most people tolerate knee MRI well. It's normal to feel anxious about medical tests, but understanding the actual risks can help put your mind at ease.
Claustrophobia and Anxiety
Early research suggests fear of enclosed spaces causes about 0.76-1.97% of MRI scans to be incomplete[Evidence: C][11][12]. About 25% of patients experience moderate to severe anxiety during scans[Evidence: C][12]. Knee MRI is typically easier than other scans because your head and chest remain outside the machine. Female patients and those entering head-first (not typical for knee scans) experience higher anxiety rates[Evidence: C][11].
Contrast Dye Safety
Research shows gadolinium-based contrast agents are safe and well tolerated[Evidence: A][5]. Acute adverse reactions are rare compared to iodinated contrast used in CT scans. Newer macrocyclic agents are safer than older linear agents[Evidence: A][5]. Research shows no proven adverse effects from small amounts of contrast that may remain in the body[Evidence: A][5]. Severe anaphylactic reactions are exceptionally rare, occurring in approximately 1 in 100,000 doses.
Who Should NOT Have a Knee MRI
- People with non-MRI-conditional pacemakers or defibrillators
- People with ferromagnetic foreign bodies in the eyes
- People with certain aneurysm clips (confirm MRI compatibility)
- People who cannot lie still for 15-45 minutes (sedation may be an option)
🥗 How to Prepare for Your Knee MRI
Before Your Appointment
- Remove metal: Take off all jewelry, watches, hearing aids, removable dental work, and hair clips before arriving
- Wear appropriate clothing: Choose loose, comfortable clothes without metal zippers, buttons, or underwire. Athletic wear or sweatpants work well.
- Review your medical history: Be prepared to answer questions about previous surgeries, implants, and allergies
- Bring prior imaging: If you have previous knee X-rays or MRIs, bring them on a CD or have them sent electronically
- Plan transportation: If sedation is needed for anxiety, arrange for someone to drive you home
- Arrive early: Plan to arrive 15-30 minutes before your scheduled appointment time
Day of the Scan
- Eating and drinking: You can eat and drink normally unless contrast or sedation is planned
- Medications: Take your regular medications unless instructed otherwise
- Empty your bladder: Use the restroom before the scan since you'll be lying still for up to 45 minutes
- Inform the technologist: Tell them about any metal implants, claustrophobia concerns, or pregnancy
Common Mistakes to Avoid
- Forgetting about metal: Even small items like bobby pins or underwire bras can cause problems. Check carefully.
- Not mentioning implants: Joint replacements are usually safe but may cause image distortion. Always disclose them.
- Moving during the scan: Even small movements blur images and may require repeat sequences. Practice lying still beforehand.
- Waiting to ask about claustrophobia options: Discuss concerns before your appointment so open MRI or sedation can be arranged.
What to Look for When Choosing a Knee MRI Provider
The quality of your test results depends on the imaging facility and radiologist who interprets your scan. Here's what to consider:
Lab Quality Markers
- CLIA certification: Clinical Laboratory Improvement Amendments accreditation is required for diagnostic imaging facilities Why it matters: Federal quality standards ensure accurate results
- ACR accreditation: American College of Radiology accreditation indicates the facility meets higher standards Why it matters: Rigorous equipment testing and quality control
- Board-certified radiologists: Verify the radiologists reading your scans are board-certified in diagnostic radiology or musculoskeletal imaging Why it matters: Specialized training improves diagnostic accuracy
- Modern equipment: Ask about the MRI scanner's field strength (1.5 Tesla or 3 Tesla preferred for detailed knee imaging) Why it matters: Higher field strength provides clearer images
- Turnaround time: Ask when results will be available (typically 24-48 hours for non-urgent scans) Why it matters: Faster results enable quicker treatment decisions
Questions to Ask Your Provider
- Is the facility ACR accredited for MRI?
- What is the field strength of the MRI scanner?
- Is an open MRI available if I'm claustrophobic?
- Do I need to fast or prepare in any specific way?
- When will results be available, and who will explain them?
- What is the cost if my insurance doesn't cover it?
- Does the facility accept my insurance?
Red Flags
- No ACR or CLIA certification: Unlicensed facilities lack quality oversight
- Unusually cheap pricing: May indicate outdated equipment or unaccredited facility
- No board-certified radiologist: Images should be interpreted by qualified specialists
- Pressure to add unnecessary scans: A knee MRI should be sufficient for most knee evaluations
How Knee MRI Compares to CT Scan and X-ray
Knee MRI, CT scan, and X-ray each have different strengths. MRI excels at visualizing soft tissues like ligaments, cartilage, and tendons, while X-rays are best for bones and CT provides detailed bone imaging with cross-sectional views. Your doctor will choose the best test based on what they need to evaluate.
| Feature | Knee MRI | CT Scan | X-ray |
|---|---|---|---|
| Best for | Soft tissues (ligaments, cartilage, tendons, meniscus) | Detailed bone imaging, complex fractures | Initial bone assessment, simple fractures |
| Soft tissue visualization | Excellent—superior to CT for soft tissue[Evidence: B][2] | Good for some soft tissues | Poor—cannot see cartilage or ligaments |
| Radiation | None—uses magnetic fields | Yes—ionizing radiation | Yes—ionizing radiation (lower dose than CT) |
| Duration | 15-45 minutes[Evidence: D][3] | 5-10 minutes | 5-10 minutes |
| ACL tear detection | Sensitivity 87%, specificity 93%[Evidence: A][1] | Limited—not primary use | Cannot detect |
| Meniscus tear detection | Sensitivity 89-92%, specificity 88-90%[Evidence: A][4] | Limited | Cannot detect |
| Cost | Higher (typically $400-$3,500) | Moderate ($200-$1,500) | Lower ($100-$500) |
| Claustrophobia concern | Yes—enclosed space (open MRI available) | Minimal—short scan, open ring design | None |
When to choose each: MRI is preferred when soft tissue injury is suspected (ACL tear, meniscus tear, cartilage damage). X-ray is typically the first test for acute knee injuries to rule out fractures. CT is used for complex fractures or when MRI is contraindicated (pacemaker, severe claustrophobia).
What The Evidence Shows (And Doesn't Show)
What Research Suggests
- Research shows knee MRI correctly identifies ACL tears in about 87% of cases (sensitivity) and correctly rules them out in 93% of cases (specificity)[Evidence: A][1]
- Research shows medial meniscus tears are detected with 89-92% sensitivity and 88-90% specificity across multiple meta-analyses[Evidence: A][1][4]
- Research shows gadolinium-based contrast agents are safe with rare acute adverse reactions[Evidence: A][5]
- Research shows claustrophobia causes only 0.76-1.97% of MRI scans to be incomplete[Evidence: C][11][12]
- Research shows AI-assisted MRI reading achieves 81% sensitivity, slightly lower than radiologists at 85%[Evidence: A][8]
What's NOT Yet Proven
- Lateral meniscus tear detection is less reliable than medial (78-80% sensitivity vs 89-92%), especially for peripheral tears
- Ramp lesions (specific tears at the back of the knee) have only 70% sensitivity, meaning arthroscopy may be needed for definitive diagnosis[Evidence: A][6]
- Long-term effects of gadolinium deposition have not been definitively studied, though current research shows no proven adverse effects[Evidence: A][5]
- Optimal imaging protocols may vary by specific condition and scanner type
Where Caution Is Needed
- About 25% of patients experience moderate to severe anxiety during MRI scans[Evidence: C][12]. Consider sedation or open MRI if you have claustrophobia.
- Metal implants can cause image artifact that limits diagnostic accuracy in the area surrounding the metal
- False negative results occur more frequently with lateral meniscus tears and peripheral horn tears
- Quality varies by facility. ACR-accredited centers with 1.5T or 3T scanners provide better image quality.
Should YOU Get a Knee MRI?
Best suited for: People with suspected ACL or meniscus tears, unexplained knee pain that hasn't responded to conservative treatment, pre-surgical planning, or when X-rays are inconclusive
Not recommended for: People with non-MRI-conditional pacemakers, ferromagnetic foreign bodies in eyes, or certain aneurysm clips. Relative caution for severe kidney disease if contrast is needed.
Realistic timeline: Scan takes 15-45 minutes. Results typically available within 24-48 hours. Total appointment time is 45-65 minutes.
When to consult a professional: Talk to your doctor before scheduling if you have any metal implants, pacemaker, claustrophobia, kidney problems, or are pregnant. Your doctor can help determine if MRI is the right test and prepare you for the experience.
Frequently Asked Questions
How much does a knee MRI cost?
Knee MRI costs vary widely depending on your location, facility type, and insurance coverage. Self-pay prices typically range from $400 to $3,500. Hospital-based facilities tend to charge more than independent imaging centers. With insurance, your out-of-pocket cost depends on your deductible and coinsurance. Medicare typically covers medically necessary knee MRIs, though prior authorization may be required. Contact your insurance company and the imaging facility for specific pricing before your appointment.
How accurate is a knee MRI for meniscus tears?
Research shows knee MRI correctly identifies medial meniscus tears in 89-92% of cases when the tear is present (sensitivity) and correctly rules them out in 88-90% of cases when no tear exists (specificity). Lateral meniscus tears have slightly lower detection rates, with sensitivity around 78-80% and specificity of 95%. Peripheral tears in the outer zone may have higher false negative rates. For certain complex tears like ramp lesions, arthroscopy may be recommended for definitive diagnosis.
Can kids have a knee MRI?
Yes. Studies suggest MRI is reliable for diagnosing knee injuries in children with acute ACL tears and works well for children ages 6-17 whose bones are still growing. The test has high accuracy for detecting cartilage injuries that occur alongside ACL tears in pediatric patients. Younger children may need sedation to remain still during the scan. Discuss your child's specific needs with your pediatric orthopedist.
Do metal implants affect knee MRI?
Most modern joint replacements, surgical screws, and plates are MRI-safe and will not be affected by the magnetic field. However, they can cause image distortion (artifact) in the area surrounding the metal, which may limit the radiologist's ability to see certain structures. Always inform your technologist about any implants so they can use techniques to minimize artifacts. Pacemakers, cochlear implants, and certain aneurysm clips may be contraindicated. The imaging facility will verify safety before your scan.
Can I drive after a knee MRI?
Yes, you can drive yourself home after a standard knee MRI without sedation. The scan does not affect your ability to drive. However, if you receive sedation for anxiety or claustrophobia, you must arrange for someone else to drive you home. The sedation effects typically last 2-4 hours and impair your ability to drive safely. Check with your facility about their sedation policy.
How soon can I get knee MRI results?
Results timing depends on the facility and urgency. Routine results are typically available within 24-48 hours. A radiologist reviews the images and creates a written report, which is sent to your ordering physician. Your doctor then explains the findings to you. Some facilities offer patient portal access where you can view reports online. Urgent cases may receive same-day interpretation. Ask your facility about their typical turnaround time.
What can a knee MRI detect that an X-ray cannot?
Knee MRI detects soft tissue injuries that are invisible on X-ray, including: ACL, PCL, MCL, and LCL ligament tears; meniscus tears; cartilage damage; tendon injuries; bone marrow edema (swelling inside the bone); cysts and tumors; inflammation and fluid accumulation; infections; and nerve abnormalities. Early research suggests nerve problems are detected in about 6 out of 1,000 routine knee scans. X-rays only show bones clearly and cannot visualize ligaments, cartilage, or tendons.
Does Medicare cover knee MRI?
Medicare typically covers medically necessary knee MRIs when ordered by a physician to diagnose or evaluate a condition. Coverage falls under Medicare Part B (outpatient services). You will generally pay 20% of the Medicare-approved amount after meeting your annual Part B deductible. Prior authorization may be required. The amount you pay depends on whether the facility accepts Medicare assignment. Contact Medicare or your Medicare Advantage plan for specific coverage details.
Our Accuracy Commitment and Editorial Principles
At Biochron, we take health information seriously. Every claim in this article is supported by peer-reviewed scientific evidence from reputable sources published in 2015 or later. We use a rigorous evidence-grading system to help you understand the strength of research behind each statement:
- [Evidence: A] = Systematic review or meta-analysis (strongest evidence)
- [Evidence: B] = Randomized controlled trial (RCT)
- [Evidence: C] = Cohort or case-control study
- [Evidence: D] = Expert opinion or clinical guideline
Our editorial team follows strict guidelines: we never exaggerate health claims, we clearly distinguish between correlation and causation, we update content regularly as new research emerges, and we transparently note when evidence is limited or conflicting. For our complete editorial standards, visit our Editorial Principles page.
This article is for informational purposes only and does not constitute medical advice. Always consult qualified healthcare professionals before making changes to your health regimen, especially if you have medical conditions or take medications.
References
- 1 . A systematic review and meta-analysis of the diagnostic accuracy of MRI for suspected ACL and meniscal tears of the knee, Phelan N, et al., Knee Surgery, Sports Traumatology, Arthroscopy, 2016, PubMed [Evidence: A]
- 2 . Diagnostic Accuracy of MRI in Knee Meniscus Tear and ACL Injury, Zhang X, et al., Alternative Therapies in Health and Medicine, 2024, PubMed [Evidence: B]
- 3 . ESR essentials: MRI of the knee-practice recommendations by ESSR, Parkar AP, Adriaensen MEAPM, European Radiology, 2024, PubMed [Evidence: D]
- 4 . Accuracy of MRI Diagnosis of Meniscal Tears of the Knee: A Meta-Analysis and Systematic Review, Wang W, et al., The Journal of Knee Surgery, 2021, PubMed [Evidence: A]
- 5 . Update on Gadolinium-Based Contrast Agent Safety, From the AJR Special Series on Contrast Media, Starekova J, et al., AJR American Journal of Roentgenology, 2024, PubMed [Evidence: A]
- 6 . Evaluating the Diagnostic Performance of MRI for Identification of Meniscal Ramp Lesions in ACL-Deficient Knees, Moteshakereh SM, et al., The Journal of Bone and Joint Surgery, 2024, PubMed [Evidence: A]
- 7 . Sensitivity and Specificity of MRI in Diagnosing Concomitant Meniscal Injuries With Pediatric and Adolescent Acute ACL Tears, Dawkins BJ, et al., Orthopaedic Journal of Sports Medicine, 2022, PubMed [Evidence: B]
- 8 . Diagnosis of knee meniscal injuries using artificial intelligence: A systematic review and meta-analysis, Mohammadi S, et al., PLoS ONE, 2025, PubMed [Evidence: A]
- 9 . Routine knee MRI: how common are peripheral nerve abnormalities, and why does it matter?, Dalili D, et al., Skeletal Radiology, 2021, PubMed [Evidence: C]
- 10 . Magnetic resonance imaging of the knee: An overview and update of conventional and state of the art imaging, Nacey NC, et al., Journal of Magnetic Resonance Imaging, 2017, PubMed [Evidence: C]
- 11 . Review of claustrophobia incidence in MRI: A service evaluation of current rates across a multi-centre service, Hudson DM, et al., Radiography, 2022, PubMed [Evidence: C]
- 12 . Prevalence and Financial Impact of Claustrophobia, Anxiety, Patient Motion, and Other Patient Events in Magnetic Resonance Imaging, Nguyen XV, et al., Topics in Magnetic Resonance Imaging, 2020, PubMed [Evidence: C]
Medical Disclaimer
This content is for informational and educational purposes only. It is not intended to provide medical advice or to take the place of such advice or treatment from a personal physician. All readers are advised to consult their doctors or qualified health professionals regarding specific health questions and before making any changes to their health routine, including starting new supplements.
Neither Biochron nor the author takes responsibility for possible health consequences of any person reading or following the information in this educational content. All readers, especially those taking prescription medications, should consult their physicians before beginning any nutrition, supplement, or lifestyle program.
If you have a medical emergency, call your doctor or emergency services immediately.






