
💡 What You Need to Know Right Away
A spine MRI is an imaging test that uses magnetic fields and radio waves to create detailed pictures of your spine, spinal cord, discs, and nerves without radiation, helping doctors detect herniated discs, nerve compression, spinal stenosis, tumors, infections, and fractures.
Also known as: Magnetic Resonance Imaging of the Spine, Spinal MRI, Lumbar Spine MRI, Cervical Spine MRI, Thoracic Spine MRI, MR Spine
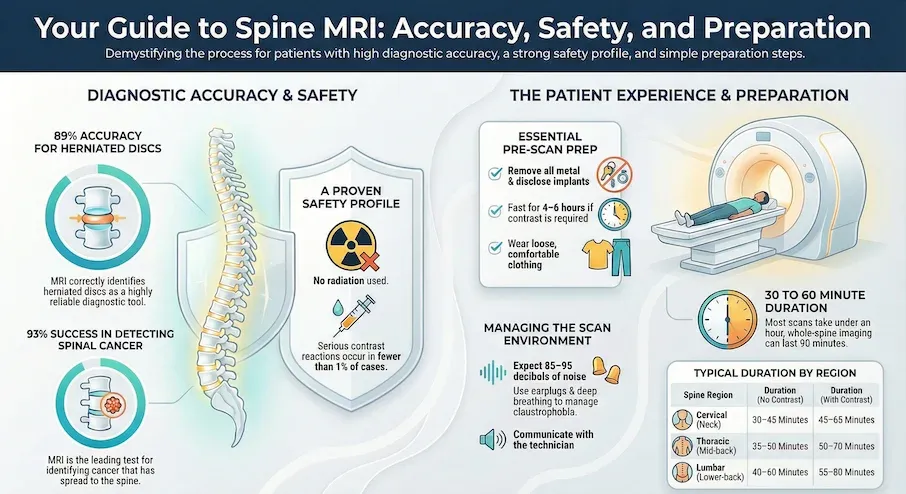
- Research shows MRI correctly identified herniated discs in about 89 out of 100 cases[Evidence: A][6]
- Clinical guidelines indicate unwanted reactions to gadolinium contrast occur in fewer than 1 out of 100 cases[Evidence: D][7]
- Research shows MRI is the best imaging test for finding cancer that has spread to the spine, correctly detecting cancer in about 93 out of 100 patients[Evidence: A][8]
- Studies suggest this shortened scan correctly identified spinal cord compression in all cases tested and correctly ruled it out in about 99 out of 100 cases[Evidence: B][1]
If your doctor has recommended a spine MRI, you probably have questions about what to expect. It is common to feel anxious about medical imaging tests, especially one that involves lying still in a tube-shaped machine for 30 to 60 minutes. The good news is that spine MRI is painless, uses no radiation, and provides your doctor with detailed images that other tests simply cannot match.
This guide walks you through everything you need to know: how to prepare, what happens during the scan, how to manage claustrophobia, what your results mean, and when you should be concerned. Whether you are dealing with back pain, neck pain, numbness, or your doctor suspects a specific condition, understanding the spine MRI process can help ease your mind.
❓ Quick Answers
What is a spine MRI?
A spine MRI is an imaging test that uses magnetic fields and radio waves to create detailed pictures of your spine, spinal cord, discs, and nerves. Unlike X-rays or CT scans, MRI uses no radiation. The scan helps doctors diagnose herniated discs, spinal stenosis, tumors, infections, and nerve compression. Research shows MRI is essential for diagnosing acute spinal cord injuries and helps doctors decide if emergency surgery is needed[Evidence: A][3].
How long does a spine MRI take?
A spine MRI typically takes 30 to 60 minutes depending on the scan area. Cervical spine scans take 30-45 minutes, thoracic spine 35-50 minutes, and lumbar spine 40-60 minutes. Whole spine imaging takes 60-90 minutes. If contrast dye is used, add 15-30 minutes. Research shows shortened protocols can reduce scan time while maintaining diagnostic accuracy[Evidence: B][1].
What does a spine MRI show?
A spine MRI shows detailed images of your vertebrae, spinal cord, discs, nerves, and surrounding soft tissues. In people with acute spinal cord injuries, this scan detected cord compression in about 7 out of 10 cases[Evidence: C][2]. Research shows MRI provides better images of spinal cord damage compared to other imaging tests[Evidence: A][3].
Is spine MRI safe?
Yes, spine MRI is very safe. The scan uses no radiation, and clinical guidelines indicate gadolinium contrast has proven extraordinarily safe after more than 30 years of use in millions of patients[Evidence: D][7]. No unwanted side effects were reported from MRI in people with spinal cord injuries[Evidence: C][2].
Can you eat before a spine MRI?
For most spine MRI scans, you can eat and drink normally beforehand. However, fasting for 4-6 hours is required if contrast dye will be used or if sedation is needed. Always follow your imaging facility's specific preparation instructions provided when you schedule your appointment.
How much does a spine MRI cost?
Spine MRI costs vary widely based on location, facility type, and insurance coverage. Lumbar spine MRI typically costs $650-$1,000 without contrast. Cervical spine costs $400-$900, thoracic $700-$1,200, and whole spine $1,500-$2,400. Adding contrast increases cost by $300-$500. Contact your imaging center for current pricing.
Is spine MRI safe for kids?
Yes, spine MRI is safe for children. The scan uses no radiation, so it can be repeated safely when needed. Research spanning 40 years shows no harmful effects from the magnetic field or radio waves. Young children may need mild sedation to stay still during the 30-60 minute scan, but this is carefully monitored by trained staff. It is common for parents to worry about imaging tests for their children.
Is spine MRI safe during pregnancy?
MRI without contrast is generally considered safe during pregnancy, though doctors typically avoid imaging during the first trimester unless absolutely necessary. Clinical guidelines indicate newer gadolinium contrast agents may be used after weighing risks and benefits[Evidence: D][12]. Always inform your doctor if you are or might be pregnant.
Spine MRI
Magnetic Resonance Imaging (MRI) uses powerful magnets and radio waves to create detailed images of the spinal anatomy, helping doctors diagnose causes of back pain without radiation.
🔬 How Does Spine MRI Work?
Understanding how MRI works can help ease anxiety about the procedure. Think of MRI like a very powerful camera that takes pictures using magnets instead of light. Your body contains billions of hydrogen atoms, mostly in water. When you lie inside the MRI machine, its powerful magnet aligns these hydrogen atoms like tiny compass needles pointing north.
The machine then sends radio waves through your body. These radio waves briefly knock the hydrogen atoms out of alignment, like flicking a compass needle. As the atoms snap back into place, they release energy signals. Different tissues release different signals. The computer captures these signals and transforms them into detailed cross-sectional images of your spine.
Why MRI excels at spine imaging: Studies suggest MRI provides clearer images of soft tissues in the spine compared to CT scans[Evidence: B][5]. This makes MRI particularly valuable for visualizing:
- Intervertebral discs – Research shows MRI correctly identified herniated discs in about 89 out of 100 cases when the condition was present[Evidence: A][6]
- Spinal cord and nerves – Research shows MRI provides better images of spinal cord damage compared to other imaging tests[Evidence: A][3]
- Vertebral tumors – In people being checked for spine cancer spread, MRI correctly detected cancer in about 93 out of 100 patients[Evidence: A][8]
- Infections – In people with spinal tuberculosis, this scan correctly detected TB features in over 97 out of 100 confirmed cases[Evidence: B][4]
Advanced detection capabilities: Studies suggest computer analysis of MRI scans detected spinal canal narrowing more accurately than radiologists, correctly identifying it in about 97 out of 100 cases[Evidence: B][9]. Research shows computer-assisted analysis of MRI scans outperforms traditional methods in accuracy, correctly identifying spine problems in about 72 to 99 out of 100 cases depending on the specific condition[Evidence: A][13].
With Contrast vs Without Contrast
Sometimes your doctor orders a spine MRI "with contrast." This means you receive an injection of a contrast agent called gadolinium into a vein in your arm. Think of contrast like adding food coloring to water. It makes certain structures and abnormalities show up more clearly on the images.
Contrast is typically used when doctors need to:
- Distinguish between scar tissue and new disc herniation after surgery
- Identify tumors or infections more clearly
- Evaluate blood vessel abnormalities
- Assess inflammation in the spine
🧪 What to Expect: The Real User Experience
During the Procedure
You will lie on a padded table that slides into a tube-shaped scanner about 23-26 inches wide. The room is kept cool at 65-68°F to prevent equipment overheating. Many patients feel cold, especially during longer scans. You will wear a hospital gown with no metal snaps, or loose clothing without metal. Blankets are available but may interfere with coil placement depending on the scan region.
For spine scans, your entire body is typically inside the tunnel. Your head may be outside the tunnel for lumbar-only scans with feet-first positioning, but inside for cervical or thoracic scans. Some machines have a mirror attached above your eyes so you can see outside the room. The space can trigger claustrophobia in approximately 15% of patients.
The machine makes loud knocking, tapping, thumping, and buzzing sounds during imaging sequences, measured at 85-95 decibels (similar to a lawn mower). Earplugs or headphones with music reduce noise by 20-30 decibels. Even with ear protection, sounds remain noticeable. Patients describe it as startling the first few times, then rhythmic and tolerable.
What You Will Feel After
Most patients have no immediate physical effects from the magnetic field or radio waves. The most common complaint is muscle stiffness from lying still, particularly in the neck, shoulders, lower back, and hips. Mild soreness typically resolves within hours. If contrast was used, you may experience mild arm soreness at the IV site (10-20% of patients) and rare bruising. Temporary ear ringing is possible if earplugs were not worn properly.
How to Make It Easier
- Before arriving: Use the bathroom immediately before the scan. Avoid caffeine 2-3 hours before to reduce jitteriness.
- For the noise: Ask for earplugs or headphones with music. Ensure earplugs are inserted properly by twisting while inserting.
- If claustrophobic: Close your eyes before the table slides into the tunnel. Request feet-first positioning for lumbar scans. Ask about open MRI options at your facility.
- During the scan: Practice deep, slow belly breathing (4 counts in, 4 counts hold, 6 counts out). Mental visualization helps time pass faster.
- Communication: You will hold a squeeze ball or panic button. Squeezing alerts the technologist immediately and pauses the scan. Early research suggests clear communication is critical for helping anxious patients complete MRI scans[Evidence: C][15].
📊 How to Prepare for Your Spine MRI
Proper preparation ensures clear images and a smooth experience. Follow these steps before your appointment.
| Preparation Step | Details | Timing |
|---|---|---|
| Remove metal objects | Jewelry, watches, hairpins, belt buckles, hearing aids, removable dental work | Before entering scan room |
| Disclose implanted devices | Pacemakers, joint replacements, cochlear implants, surgical clips, metal fragments | When scheduling and at check-in |
| Inform about pregnancy | Tell staff if you are or might be pregnant | When scheduling |
| Fast if required | 4-6 hours before if contrast ordered or sedation needed | Day of appointment |
| Arrange transportation | If sedation used, you cannot drive for 24 hours | Day of appointment |
| Wear appropriate clothing | Loose, comfortable clothing without metal. You may change into hospital gown. | Day of appointment |
| Arrive early | Complete paperwork and screening questionnaire | 15 minutes before appointment |
Scan Duration by Region
| Scan Type | Duration Without Contrast | Duration With Contrast |
|---|---|---|
| Cervical spine (C1-C7) | 30-45 minutes | 45-65 minutes |
| Thoracic spine (T1-T12) | 35-50 minutes | 50-70 minutes |
| Lumbar spine (L1-L5) | 40-60 minutes | 55-80 minutes |
| Whole spine | 60-90 minutes | 80-120 minutes |
⚠️ Safety, Risks, and Contraindications
The test itself is painless and uses no radiation. Most people tolerate MRI well. It is normal to feel anxious about medical tests. Understanding the safety profile can help ease concerns.
Contrast Agent Safety
If your MRI requires contrast, you will receive an injection of gadolinium-based contrast agent. Clinical guidelines indicate unwanted reactions to gadolinium contrast occur in fewer than 1 out of 100 cases, with serious reactions being extremely rare[Evidence: D][7].
Clinical guidelines indicate the serious condition called NSF (nephrogenic systemic fibrosis) has been virtually eliminated when using newer group II gadolinium agents[Evidence: D][7]. Research shows zero cases of NSF occurred in nearly 5,000 contrast administrations to people with severe kidney disease when using newer agents[Evidence: A][11].
Who Should Not Have a Spine MRI
- Ferromagnetic brain aneurysm clips: The magnetic field could move the clip
- Older pacemakers or defibrillators: Many newer devices are MRI-conditional. Always disclose all implants to your technologist.
- Metal fragments in eyes: Previous welding or metalwork without eye protection may have left metal fragments
- Cochlear implants: Some older models are not MRI-compatible
Special Populations
Pregnancy: MRI without contrast is generally considered safe during pregnancy, though doctors typically avoid first-trimester imaging unless medically necessary. Clinical guidelines indicate newer gadolinium contrast agents may be used in pregnancy after careful risk-benefit assessment[Evidence: D][12].
Kidney disease: Clinical guidelines indicate newer gadolinium contrast agents may be used in people with advanced kidney disease after weighing risks and benefits[Evidence: D][12]. Research shows the risk of NSF with newer gadolinium agents in people with severe kidney disease is essentially zero, with risk less than 1 in 1,000[Evidence: A][11].
🥗 Practical Guidance for Your Spine MRI
Managing Claustrophobia
Early research suggests specific coping strategies help people with claustrophobia complete MRI scans successfully[Evidence: C][15]. Early research suggests virtual reality preparation and clear communication help anxious patients complete MRI scans[Evidence: C][15].
Strategies that help:
- Ask about open MRI options (wider bore, less confined)
- Request feet-first positioning for lumbar scans
- Keep eyes closed throughout the scan
- Use the provided headphones with music
- Practice breathing exercises before your appointment
- Ask your doctor about mild sedation (Valium, Ativan) for severe anxiety
Getting Your Results
After your scan completes, a radiologist (a doctor who specializes in reading medical images) reviews your images and creates a report. This typically takes 1-2 days. The report is sent to the doctor who ordered your MRI, who will contact you to discuss findings, usually within 1-2 weeks unless results are urgent.
Research shows changes seen on MRI scans help predict how well people will recover after spinal cord injury[Evidence: A][3].
Understanding Common Findings
Many MRI findings are normal parts of aging and do not cause symptoms:
- Disc bulge: The disc cushion pushes out slightly (common after age 40)
- Disc desiccation: The disc has lost moisture (normal aging)
- Osteophytes: Small bone spurs (common with age)
- Facet arthropathy: Wear in the small joints of the spine
What to Look for When Choosing a Spine MRI Provider
The quality of your test results depends on the lab and healthcare provider. Here is what to consider:
Lab Quality Markers
- CLIA certification: Clinical Laboratory Improvement Amendments accreditation required Why it matters: Federal quality standards ensure accurate results
- ACR accreditation: American College of Radiology certification indicates high standards Why it matters: ACR-accredited facilities meet rigorous equipment and personnel standards
- Board-certified radiologists: Verify radiologists are board-certified in diagnostic radiology Why it matters: Specialized training improves interpretation accuracy
- Modern equipment: 1.5 Tesla or 3 Tesla MRI scanners Why it matters: Higher field strength provides better image detail
Questions to Ask Your Provider
- Is your facility ACR-accredited for MRI?
- What type of MRI scanner do you use (open vs closed, Tesla strength)?
- Do you offer open MRI for claustrophobic patients?
- When will results be available?
- What is the cost if my insurance does not cover it?
- Who will explain my results?
Red Flags
- No ACR accreditation: Non-accredited facilities lack quality oversight
- Unusually cheap pricing: May indicate older equipment or unaccredited facility
- Long wait times for results: Quality facilities provide results within 1-3 days
- No radiologist available to discuss results: You should have access to expert interpretation
Spine MRI vs CT Scan: What is the Difference?
MRI and CT scans both create detailed images of your spine, but they work through different mechanisms and excel at different tasks. Your doctor chooses the appropriate test based on what they need to see.
| Feature | Spine MRI | CT Scan |
|---|---|---|
| Radiation | None (uses magnetic fields) | Yes (uses X-rays) |
| Soft Tissue Detail | Excellent. Studies suggest MRI provides clearer images of soft tissues in the spine compared to CT scans[Evidence: B][5] | Good |
| Bone Detail | Good | Excellent |
| Disc Herniation Accuracy | In people with herniated discs, MRI correctly identified the condition in about 92 out of 100 cases and correctly ruled it out in all cases tested[Evidence: B][5] | CT scans were less accurate, with about 83 out of 100 for detection and about 71 out of 100 for ruling out[Evidence: B][5] |
| Duration | 30-60 minutes | 5-10 minutes |
| Best For | Disc problems, nerve compression, spinal cord injuries, tumors, infections | Fractures, bone problems, trauma assessment, patients with MRI contraindications |
| Claustrophobia Concern | Yes (enclosed tube for 30-60 minutes) | Less (open ring, quick scan) |
Clinical guidelines recommend MRI as the first imaging test for people considering surgery after 6 weeks of conservative treatment for low back pain[Evidence: D][10]. Your doctor will determine which test is most appropriate for your specific situation.
What The Evidence Shows (And Does Not Show)
What Research Suggests
- Research shows MRI correctly identified herniated discs in about 89 out of 100 cases (38 studies, 1,875 patients analyzed)[Evidence: A][6]
- In people being checked for spine cancer spread, MRI correctly detected cancer in about 93 out of 100 patients and correctly ruled it out in about 85 out of 100 patients[Evidence: A][8]
- Studies suggest shortened scan protocols correctly identified spinal cord compression in all cases tested (sensitivity 100%, 95% CI 96-100%) and correctly ruled it out in about 99 out of 100 cases (specificity 98.6%)[Evidence: B][1]
- Clinical guidelines indicate gadolinium contrast has proven extraordinarily safe after more than 30 years of use, with acute adverse reactions in fewer than 1 out of 100 cases (0.45%)[Evidence: D][7]
- Research shows zero cases of NSF occurred in nearly 5,000 contrast administrations to people with severe kidney disease when using newer group II agents[Evidence: A][11]
What is NOT Yet Proven
- Optimal imaging protocols for all spine conditions vary, and no single protocol is universally superior
- Long-term effects of repeated MRI scans have not been extensively studied, though no adverse effects have been identified in 40+ years of use
- The clinical significance of many MRI findings (such as disc bulges in asymptomatic people) remains debated
- Whether AI-assisted interpretation will fully replace radiologist review requires further validation
Where Caution Is Needed
- Patients with non-MRI-conditional implanted devices should not undergo MRI without cardiology clearance
- Claustrophobia affects approximately 15% of patients and may prevent scan completion without sedation or open MRI
- Gadolinium contrast should be used cautiously in patients with severe kidney disease, though clinical guidelines indicate newer agents may be used after risk-benefit assessment[Evidence: D][12]
- First-trimester pregnancy imaging is generally avoided unless medically necessary
Should YOU Get a Spine MRI?
Best suited for: People with persistent back or neck pain, numbness, weakness, or suspected disc problems, stenosis, tumors, or infections after initial evaluation by a physician
Not recommended for: People with ferromagnetic implants, non-MRI-conditional pacemakers, or metallic eye foreign bodies. Those with severe claustrophobia may need sedation or open MRI alternatives.
Realistic timeline: Scan takes 30-90 minutes. Results typically available in 1-2 days. Follow-up with ordering physician in 1-2 weeks unless urgent.
When to consult a professional: Always obtain spine MRI through a physician's order. Discuss whether MRI is appropriate for your specific symptoms and medical history.
Frequently Asked Questions
What is the difference between spine MRI with contrast and without contrast?
MRI without contrast is the standard scan using only magnetic fields. MRI with contrast involves injecting gadolinium dye into your vein before or during the scan. Contrast makes certain abnormalities more visible, particularly tumors, infections, inflammation, and post-surgical changes. Clinical guidelines indicate unwanted reactions to gadolinium contrast occur in fewer than 1 out of 100 cases. Your doctor decides if contrast is needed based on what they are looking for.
Can you have a spine MRI with a pacemaker?
Many newer pacemakers and defibrillators are MRI-conditional, meaning scans are safe under specific protocols. However, older devices may not be compatible with MRI's strong magnetic field. Always disclose all implanted devices to the MRI technologist, who will verify safety with your cardiologist and device manufacturer. If approved, the pacemaker will be temporarily reprogrammed before the scan. Never assume your device is safe. Always bring your device identification card.
Can you have a spine MRI with metal implants?
Most modern orthopedic implants (joint replacements, spinal hardware, plates, screws) are made from non-ferromagnetic materials and are MRI-safe. However, you must disclose all implants to your technologist, including the type, location, and when it was implanted. Some older implants or specialty devices may not be compatible. The imaging facility will verify safety before proceeding.
What is an open MRI?
An open MRI uses a different machine design with open sides rather than a closed tube. This design reduces claustrophobia and accommodates larger patients. Open MRI machines typically use lower magnetic field strength (0.3-1.0 Tesla vs 1.5-3.0 Tesla for closed MRI), which may result in slightly less detailed images for some conditions. Ask your facility if open MRI is available and appropriate for your diagnostic needs.
How accurate is a spine MRI?
Research shows MRI demonstrates excellent overall performance for diagnosing herniated discs. Research shows MRI correctly identified herniated discs in about 89 out of 100 cases when the condition was present. When looking at individual bone lesions for cancer spread, MRI correctly identified cancer in about 91 out of 100 lesions and correctly ruled it out in about 94 out of 100 lesions.
When do you need a spine MRI?
Clinical guidelines recommend MRI as the appropriate test for people with low back pain when cauda equina syndrome is suspected. Common reasons for spine MRI include persistent back or neck pain not responding to treatment, leg or arm weakness or numbness, suspected herniated disc, spinal stenosis evaluation, pre-surgical planning, post-surgical assessment, and suspected tumors or infections.
Will a spine MRI hurt?
The MRI scan itself is completely painless. You will not feel the magnetic field or radio waves. However, lying completely still for 30-90 minutes can cause muscle stiffness, especially in patients with existing back pain. Hip or shoulder discomfort is common. If contrast is used, you will feel a brief needle stick for IV insertion and possibly a cool sensation as contrast enters your bloodstream. Request extra padding under your knees or lower back if you have chronic pain.
How long does it take to get spine MRI results?
After your scan completes, a radiologist reviews your images and creates a report, typically within 1-2 days. The report is sent to the doctor who ordered your MRI, who will contact you to discuss findings, usually within 1-2 weeks unless results are urgent. If you have an online patient portal, results may appear there once your doctor reviews them. For urgent concerns, contact your ordering physician directly.
Can you have a spine MRI if you are claustrophobic?
Yes, many claustrophobic patients successfully complete spine MRI scans using coping strategies. Early research suggests specific coping strategies help people with claustrophobia complete MRI scans successfully. Options include open MRI machines, sedation medication, feet-first positioning, keeping eyes closed, using headphones with music, and breathing exercises. Discuss your concerns with your doctor before scheduling.
Do you need to remove jewelry for spine MRI?
Yes, remove all metal objects before entering the MRI room. This includes jewelry, watches, hairpins, belt buckles, hearing aids, removable dental work, and eyeglasses. The powerful magnetic field can pull on metal objects, potentially causing injury. Metal objects also create artifacts that distort images. You will complete a detailed screening questionnaire and may walk through a metal detector before your scan.
Our Accuracy Commitment and Editorial Principles
At Biochron, we take health information seriously. Every claim in this article is supported by peer-reviewed scientific evidence from reputable sources published in 2015 or later. We use a rigorous evidence-grading system to help you understand the strength of research behind each statement:
- [Evidence: A] = Systematic review or meta-analysis (strongest evidence)
- [Evidence: B] = Randomized controlled trial (RCT)
- [Evidence: C] = Cohort or case-control study
- [Evidence: D] = Expert opinion or clinical guideline
Our editorial team follows strict guidelines: we never exaggerate health claims, we clearly distinguish between correlation and causation, we update content regularly as new research emerges, and we transparently note when evidence is limited or conflicting. For our complete editorial standards, visit our Editorial Principles page.
This article is for informational purposes only and does not constitute medical advice. Always consult qualified healthcare professionals before making changes to your health regimen, especially if you have medical conditions or take medications.
References
- 1 . Shortened total spine MRI protocol in the detection of spinal cord compression and pathology for emergent settings: a noninferiority study, Chang YM et al., Emergency radiology, 2022, PubMed [Kanıt: B]
- 2 . The Role of MRI in Evaluating Spinal Cord Injuries: Diagnostic Accuracy, Prognostic Value, and Clinical Decision-Making, Agha Tabari K et al., Cureus, 2025, PubMed [Kanıt: C]
- 3 . The Role of Magnetic Resonance Imaging to Inform Clinical Decision-Making in Acute Spinal Cord Injury: A Systematic Review and Meta-Analysis, Ghaffari-Rafi A et al., Journal of clinical medicine, 2021, PubMed [Kanıt: A]
- 4 . Diagnostic accuracy of whole spine magnetic resonance imaging in spinal tuberculosis validated through tissue studies, Kanna RM et al., European spine journal, 2019, PubMed [Kanıt: B]
- 5 . Diagnostic accuracy of lumbar CT and MRI in the evaluation of chronic low back pain without red flag symptoms, Martel Villagrán J et al., Radiologia, 2023, PubMed [Kanıt: B]
- 6 . Value of imaging examinations in diagnosing lumbar disc herniation: A systematic review and meta-analysis, Huang Z et al., Frontiers in surgery, 2023, PubMed [Kanıt: A]
- 7 . Update on Gadolinium-Based Contrast Agent Safety, From the AJR Special Series on Contrast Media, Starekova J et al., AJR. American journal of roentgenology, 2024, PubMed [Kanıt: D]
- 8 . Detection of vertebral metastases: a meta-analysis comparing MRI, CT, PET, BS and BS with SPECT, Liu T et al., Journal of cancer research and clinical oncology, 2017, PubMed [Kanıt: A]
- 9 . A neural network model for detection and classification of lumbar spinal stenosis on MRI, Tumko V et al., European spine journal, 2024, PubMed [Kanıt: B]
- 10 . ACR Appropriateness Criteria® Low Back Pain: 2021 Update, Expert Panel on Neurological Imaging et al., Journal of the American College of Radiology, 2021, PubMed [Kanıt: D]
- 11 . Risk of Nephrogenic Systemic Fibrosis in Patients With Stage 4 or 5 Chronic Kidney Disease Receiving a Group II Gadolinium-Based Contrast Agent: A Systematic Review and Meta-analysis, Woolen SA et al., JAMA internal medicine, 2020, PubMed [Kanıt: A]
- 12 . Use of Intravenous Gadolinium-based Contrast Media in Patients with Kidney Disease: Consensus Statements from the American College of Radiology and the National Kidney Foundation, Weinreb JC et al., Radiology, 2021, PubMed [Kanıt: D]
- 13 . Artificial Intelligence-Assisted MRI Diagnosis in Lumbar Degenerative Disc Disease: A Systematic Review, Liawrungrueang W et al., Global spine journal, 2025, PubMed [Kanıt: A]
- 14 . Deep learning-based high-accuracy detection for lumbar and cervical degenerative disease on T2-weighted MR images, Yi W et al., European spine journal, 2023, PubMed [Kanıt: B]
- 15 . Supporting claustrophobic patients during Magnetic Resonance Imaging examination- the patient perspective, Lawal O et al., Radiography, 2023, PubMed [Kanıt: C]
Medical Disclaimer
This content is for informational and educational purposes only. It is not intended to provide medical advice or to take the place of such advice or treatment from a personal physician. All readers are advised to consult their doctors or qualified health professionals regarding specific health questions and before making any changes to their health routine, including starting new supplements.
Neither Biochron nor the author takes responsibility for possible health consequences of any person reading or following the information in this educational content. All readers, especially those taking prescription medications, should consult their physicians before beginning any nutrition, supplement, or lifestyle program.
If you have a medical emergency, call your doctor or emergency services immediately.






