Health Guide
Psoriasis Natural Remedies: Anti-Inflammatory Diet, Gut Health & Triggers

💡 What You Need to Know Right Away
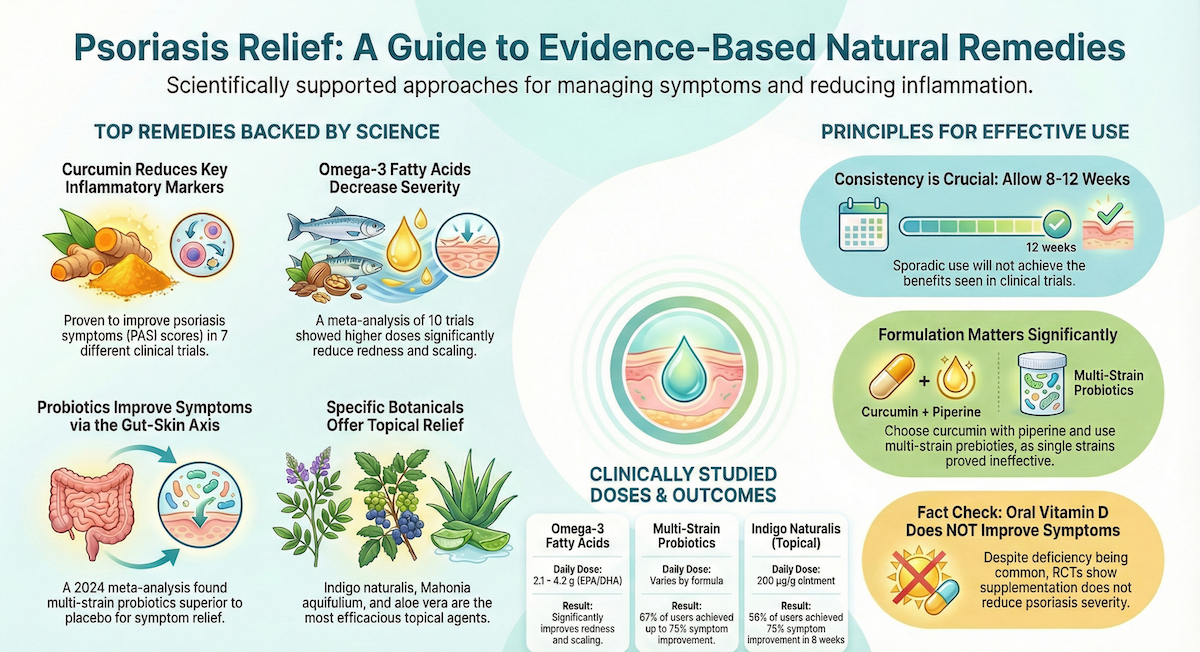
- Curcumin improves psoriasis symptoms: Both monotherapy and combination therapy improved PASI scores compared to controls across 7 clinical trials.[Evidence: A][1]
- Omega-3 fatty acids reduce severity: A meta-analysis of 10 trials with 560 participants showed significant PASI score reduction, with greater effects at higher dosages.[Evidence: A][4]
- Probiotics outperform placebo: A 2024 meta-analysis of 5 RCTs found probiotics superior to placebo for PASI reduction and quality-of-life improvements.[Evidence: A][9]
- Topical botanicals show promise: Mahonia aquifolium, indigo naturalis, aloe vera, and capsaicin are the most efficacious botanical agents according to a systematic review of 27 clinical trials.[Evidence: A][14]
Living with psoriasis can feel like an endless cycle of flare-ups, frustration, and searching for relief. It is common to feel overwhelmed by conflicting information about what actually works. Many people worry about side effects from conventional treatments or simply want to explore complementary options.
The good news is that scientific research on natural remedies for psoriasis has advanced significantly. This guide examines 13 evidence-based natural treatments, from curcumin and omega-3 fatty acids to probiotics and topical botanicals. You will learn what the research actually shows, appropriate dosages studied in clinical trials, and important safety considerations. Every claim is backed by peer-reviewed evidence from systematic reviews and randomized controlled trials.
❓ Quick Answers
What is psoriasis?
Psoriasis is a chronic autoimmune disease that causes skin cells to multiply up to 10 times faster than normal. This rapid turnover leads to thick, red, scaly patches called plaques that can appear anywhere on the body but commonly affect the scalp, elbows, and knees. The condition involves systemic inflammation driven by immune dysregulation, particularly involving TNF-α, IL-17, and IL-22 cytokines.[Evidence: A][1]
How do natural remedies work for psoriasis?
Natural remedies target psoriasis through multiple mechanisms. Curcumin reduces inflammatory markers including IL-17, TNF-α, and IL-22.[Evidence: A][1] Omega-3 fatty acids decrease systemic inflammation and improve erythema and scaling.[Evidence: A][4] Probiotics modulate gut microbiota, which influences immune response through the gut-skin axis.[Evidence: A][9]
What are the benefits of natural remedies for psoriasis?
Evidence-based natural remedies offer several benefits: reduced PASI scores indicating less severe symptoms, decreased inflammation, improved quality of life, and fewer systemic side effects than conventional medications. A systematic review of 20 RCTs found herbal therapies including aloe vera, indigo naturalis, and Mahonia show therapeutic benefit for psoriasis management.[Evidence: A][7]
Is turmeric good for psoriasis?
Yes, turmeric's active compound curcumin shows clinical benefit for psoriasis. A systematic review of 26 studies (7 clinical trials, 19 preclinical) found that both curcumin monotherapy and combination therapy improved PASI scores compared to controls.[Evidence: A][1] Patient surveys report 46.4% of psoriatic arthritis patients using curcumin experienced significant pain reduction.[Evidence: D][10]
Does aloe vera help psoriasis?
Research supports aloe vera for psoriasis symptom relief. A systematic review of 27 clinical trials identified aloe vera as one of the most efficacious topical botanical agents for psoriasis, along with Mahonia aquifolium, indigo naturalis, and capsaicin.[Evidence: A][14] Aloe vera contains aloe-emodin, which has anti-inflammatory and antiproliferative properties.
How much omega-3 should I take for psoriasis?
Clinical trials used omega-3 dosages ranging from 2.1 to 4.2 grams daily. A meta-analysis of 10 RCTs found greater effects at higher dosages, with 4.2g EPA/DHA showing significant improvements in PASI scores, erythema, and scaling.[Evidence: A][4] Supplementation duration of 8 or more weeks produced measurable benefits.
Can stress cause psoriasis?
Stress does not cause psoriasis but can trigger flare-ups in people who have the condition. Stress activates inflammatory pathways that worsen psoriasis symptoms. The gut-skin axis connects psychological stress to skin inflammation through microbiome changes. Probiotic supplementation improved both PASI scores and depression symptoms in patients with plaque psoriasis.[Evidence: B][5]
Should I try natural remedies for psoriasis?
Natural remedies may complement conventional treatment under medical supervision. Systematic reviews confirm herbal interventions show therapeutic benefit, but additional rigorous research is needed.[Evidence: A][7] Natural remedies are generally safer than systemic agents during pregnancy, where topical therapies are first-line treatment.[Evidence: D][13] Discuss with your dermatologist before starting any supplement regimen.
🔬 How Do Natural Remedies Work for Psoriasis?
Understanding how natural remedies work helps you make informed decisions about which options may benefit your specific situation. Psoriasis is fundamentally an immune system disorder, and effective natural treatments work by modulating this immune dysfunction.
Think of your immune system as a security alarm that has become overly sensitive. In psoriasis, this alarm keeps going off even when there is no real threat, causing inflammation that accelerates skin cell production. Natural remedies work like calibrating that alarm back to appropriate sensitivity levels.
Anti-Inflammatory Mechanisms
Curcumin reduces inflammatory markers including IL-17, TNF-α, and IL-22, which are key cytokines driving psoriasis inflammation.[Evidence: A][1] A meta-analysis of 31 RCTs across 10 autoimmune conditions found the strongest evidence for curcumin's benefits in psoriasis, ulcerative colitis, and rheumatoid arthritis.[Evidence: A][12]
Omega-3 fatty acids, particularly EPA and DHA, decrease systemic inflammation through multiple pathways. They compete with pro-inflammatory omega-6 fatty acids and produce anti-inflammatory resolvins. A meta-analysis showed omega-3 supplementation improved erythema and scaling in psoriasis patients.[Evidence: A][4]
The Gut-Skin Axis
Your gut microbiome acts like a control center for your immune system. When gut bacteria become imbalanced, inflammatory signals travel throughout the body, including to the skin. Probiotics restore balance to this microbial community.
A 2024 meta-analysis of 5 RCTs with 286 patients confirmed probiotics are superior to placebo for PASI reduction, with statistically significant quality-of-life improvements.[Evidence: A][9] Multi-strain probiotic formulations appear more effective than single strains. One RCT found 66.7% of the probiotic group achieved up to 75% PASI improvement versus 41.9% in the placebo group.[Evidence: B][11]
Topical Botanical Mechanisms
Topical natural remedies work directly on affected skin. Tea tree oil contains terpinen-4-ol, identified as the major component with anti-inflammatory properties.[Evidence: A][15] Indigo naturalis contains indirubin, which inhibits keratinocyte proliferation. In a dose-controlled RCT, 200 μg/g indirubin concentration in ointment was most effective, with 56.3% achieving PASI 75 response at week 8 versus 0% in the placebo group.[Evidence: B][6]
Mahonia aquifolium (Oregon grape) contains berberine, an alkaloid that reduces inflammation and slows excessive skin cell growth. This botanical was identified as one of the most efficacious in a systematic review of 27 clinical trials.[Evidence: A][14]
📊 Dosage and How to Use
The following dosages come from clinical trials studying natural remedies for psoriasis. Always consult your healthcare provider before starting any supplement, especially if you take other medications.
| Remedy | Dosage | Duration | Evidence |
|---|---|---|---|
| Curcumin (oral) | 200-1000 mg/day | 8-12 weeks | [A][1][10] |
| Omega-3 fatty acids | 2.1-4.2 g/day (EPA/DHA) | 8+ weeks | [A][4] |
| Multi-strain probiotics | Per product (multi-strain formula) | 12 weeks | [B][11] |
| Indigo naturalis ointment | 200 μg/g indirubin concentration | 8 weeks (twice daily) | [B][6] |
| Herbal preparations (various) | Variable by formulation | 8-12 weeks | [A][7] |
Important Dosage Considerations
Curcumin: Patient surveys indicate dosing at 200-1000 mg daily. Consistent use over extended periods showed better results than intermittent supplementation.[Evidence: D][10] Curcumin has poor bioavailability alone. Look for formulations with piperine (black pepper extract) or phospholipid complexes to enhance absorption.
Omega-3s: Higher dosages showed greater effects in the meta-analysis. The 4.2g EPA/DHA dose produced stronger PASI improvements than lower doses.[Evidence: A][4] Take with meals containing fat to improve absorption.
Probiotics: Multi-strain formulations outperformed single-strain products. One RCT found Lactobacillus rhamnosus alone did not significantly improve psoriasis (p = 0.620), while multi-strain mixtures showed significant benefit.[Evidence: B][8][11] Allow 8-12 weeks for microbiome modulation to take effect.
⚠️ Risks, Side Effects, and Warnings
Side Effects
Common side effects of topical botanical agents include transient skin irritation.[Evidence: A][14] Indigo naturalis ointment showed no severe treatment-related adverse events in the dose-controlled trial.[Evidence: B][6] Omega-3 supplements may cause mild gastrointestinal symptoms. Curcumin is generally well-tolerated at therapeutic doses but has limited systemic absorption without bioavailability enhancers.
Drug Interactions
Omega-3 fatty acids have mild anticoagulant properties. Clinically significant bleeding risk occurs primarily with concurrent anticoagulant medications. Inform your healthcare provider of all medications before combining natural remedies with prescriptions.
Contraindications
Pregnancy and Lactation: Topical therapies including low-to-moderate potency steroids are first-line for psoriasis treatment during pregnancy. Methotrexate and acitretin are contraindicated. Natural remedies are generally safer than systemic agents.[Evidence: D][13] Consult your obstetrician before using any supplements during pregnancy.
Monitoring Recommendations
Track your symptoms during any natural remedy trial. Document PASI-like observations including redness, thickness, and scaling of affected areas. Photograph plaques weekly to assess progress objectively. If no improvement occurs after 8-12 weeks of consistent use, consult your dermatologist to reassess your treatment approach.
🥗 Practical Ways to Use Psoriasis Natural Remedies
How to Use This in Your Daily Life
Scenario 1: Reducing Overall Inflammation
- Dose: Omega-3 fatty acids 2.1-4.2g daily (EPA/DHA combined)[4]
- Duration: 8+ weeks for measurable benefit
- Population: Adults with chronic plaque psoriasis
- Timing: Take with meals containing fat
- What to track: PASI score changes, erythema, scaling
- Expected results: Improvements in erythema and scaling[Evidence: A][4]
Scenario 2: Supporting Gut-Skin Axis
- Dose: Multi-strain probiotic formula (per product instructions)[11]
- Duration: 12 weeks for microbiome modulation
- Population: Adults with plaque psoriasis
- Timing: Morning, with or without food (per product instructions)
- What to track: PASI score, quality of life, mood
- Expected results: 66.7% showed PASI improvement up to 75% in RCT[Evidence: B][11]
Scenario 3: Topical Relief for Plaques
- Dose: Indigo naturalis ointment (200 μg/g indirubin)[6]
- Duration: 8 weeks of consistent use
- Application: Twice daily to affected areas
- What to track: Plaque thickness, redness, scaling
- Expected results: 56.3% achieved PASI 75 response at week 8[Evidence: B][6]
Practical Integration
Store supplements in a cool, dry place away from direct sunlight. Omega-3 supplements may be refrigerated to prevent rancidity. Topical preparations should be stored per product label instructions.
Common Mistakes to Avoid
- Expecting immediate results: Studies used 8-12 week durations[1][7]. Sporadic use will not achieve the benefits seen in clinical trials.
- Using single-strain probiotics: Multi-strain formulations showed significant benefits while single-strain L. rhamnosus did not (p = 0.620).[8]
- Inadequate curcumin absorption: Standard curcumin has poor bioavailability. Choose formulations with piperine or phospholipid complexes.
- Stopping conventional treatment abruptly: Natural remedies complement medical care. Discontinue prescriptions only under physician supervision.
⚖️ Natural Remedies Comparison: Which Should You Try First?
Not all natural remedies have equal evidence. This comparison helps you prioritize based on research quality and practical considerations.
| Remedy | Evidence Quality | Best For | Considerations |
|---|---|---|---|
| Curcumin | [A] (7 clinical trials, meta-analysis) | Systemic inflammation, joint symptoms | Requires bioavailability enhancement[1] |
| Omega-3 fatty acids | [A] (10 RCTs, 560 participants) | Erythema, scaling, overall severity | Higher doses more effective[4] |
| Multi-strain probiotics | [A]/[B] (5 RCTs in meta-analysis) | Gut-skin axis, quality of life | Multi-strain superior to single-strain[9] |
| Indigo naturalis (topical) | [B] (dose-controlled RCT) | Localized plaque psoriasis | 56.3% PASI 75 at 8 weeks[6] |
| Vitamin D3 (oral) | [A]/[B] (negative findings) | Addressing deficiency (not symptoms) | Supplementation did not improve PASI[2][3] |
| Aloe vera, Mahonia, Capsaicin | [A] (systematic review of 27 trials) | Topical symptom relief | Most efficacious botanicals[14] |
Important Finding on Vitamin D
Despite clear evidence that psoriasis patients have significantly lower vitamin D levels than controls (21.0 ± 8.3 vs. 27.3 ± 9.8 ng/mL), oral vitamin D supplementation did not seem to improve clinical manifestations in meta-analysis.[Evidence: A][3] A JAMA Dermatology RCT found vitamin D3 100,000 IU/month did not reduce psoriasis severity compared to placebo.[Evidence: B][2] Address deficiency for overall health, but do not expect oral vitamin D to directly improve psoriasis symptoms.
What The Evidence Shows (And Doesn't Show)
What Research Suggests
- Curcumin (both monotherapy and combination therapy) improved PASI scores compared to controls across 7 clinical trials and reduced inflammatory markers IL-17, TNF-α, and IL-22[Evidence: A][1]
- Omega-3 supplementation (10 RCTs, n=560) produced significant PASI reduction with greater effects at higher dosages (up to 4.2g EPA/DHA) and improvements in erythema and scaling[Evidence: A][4]
- Probiotics (5 RCTs, n=286) are superior to placebo for PASI reduction with statistically significant quality-of-life improvements[Evidence: A][9]
- Multi-strain probiotics showed 66.7% response rate versus 41.9% placebo, with lower relapse rates at 6-month follow-up[Evidence: B][11]
- Topical indigo naturalis (200 μg/g indirubin) achieved 56.3% PASI 75 response at 8 weeks versus 0% placebo with no severe adverse events[Evidence: B][6]
What's NOT Yet Proven
- Oral vitamin D supplementation for symptom improvement: Despite clear vitamin D deficiency in psoriasis patients, supplementation did not improve PASI scores in RCTs[2][3]
- Long-term safety data beyond 12 months: Most studies lasted 8-12 weeks. Long-term efficacy and safety data are limited.
- Optimal dosing protocols: Curcumin studies used variable dosages (200-1000mg). Optimal therapeutic doses not established.
- Pediatric populations: Studies focused on adults. Safety and efficacy in children with psoriasis require additional research.
- Single-strain probiotic efficacy: L. rhamnosus alone did not show significant benefit (p=0.620)[8]
- Aloe vera and tea tree oil large-scale RCTs: While systematic reviews support their use, psoriasis-specific large-scale trials are lacking
Where Caution Is Needed
- Omega-3 fatty acids have mild anticoagulant properties. Clinically significant bleeding risk with concurrent anticoagulant medications[Evidence: A][4]
- Topical botanicals commonly cause transient skin irritation and may cause allergic sensitization[Evidence: A][14]
- Curcumin has poor bioavailability without enhancement. Standard turmeric supplements may not deliver therapeutic levels.
- Multi-strain probiotics showed benefit while single-strain did not. Formulation matters significantly for efficacy[8][11]
- Methotrexate and acitretin are contraindicated in pregnancy. Natural remedies are generally safer than systemic agents during pregnancy[Evidence: D][13]
Should YOU Try This?
Best suited for: Adults with mild-to-moderate plaque psoriasis seeking to complement conventional treatment, those interested in addressing gut health and systemic inflammation, patients who tolerate natural supplements well
Not recommended for: Individuals allergic to specific botanicals, those taking anticoagulants (use caution with omega-3), pregnant or breastfeeding women without medical supervision, anyone seeking to replace prescribed psoriasis medications without physician guidance
Realistic timeline: Clinical trials used 8-12 weeks duration. Expect to use remedies consistently for 2-3 months before evaluating effectiveness.[Evidence: A][7]
When to consult a professional: Before starting any supplement (especially with medications), if symptoms worsen despite natural remedy use, if you experience adverse reactions, and for periodic assessment of your overall psoriasis management plan
Frequently Asked Questions
Can psoriasis go away on its own?
No, psoriasis does not permanently go away on its own. It is a chronic autoimmune condition requiring ongoing management. However, spontaneous remission periods can occur, where symptoms temporarily improve without treatment. The duration and frequency of remissions vary significantly between individuals. Triggers such as stress, infections, and certain medications can cause flare-ups. Consistent use of natural remedies and lifestyle modifications may help extend remission periods. Multi-strain probiotic users showed lower relapse rates and improved responses persisting at six-month follow-up.
What vitamin deficiency causes psoriasis?
No single vitamin deficiency causes psoriasis. However, vitamin D deficiency is most strongly associated with psoriasis severity. A meta-analysis of 23 studies found psoriasis patients had significantly lower 25(OH)D levels than controls (21.0 ± 8.3 vs. 27.3 ± 9.8 ng/mL). Importantly, deficiency does not cause psoriasis. It may worsen symptoms in those who already have the condition. Correcting deficiency supports overall health, but oral vitamin D supplementation alone does not significantly improve PASI scores based on RCT evidence.
What foods make psoriasis worse?
Pro-inflammatory foods may worsen psoriasis symptoms. These include highly processed foods, refined sugars, saturated fats, and excessive alcohol. Individual triggers vary. Psoriasis involves systemic inflammation, and diet influences inflammatory markers. An anti-inflammatory diet emphasizing omega-3 fatty acids showed clinical benefits. A meta-analysis of 10 RCTs demonstrated that omega-3 supplementation improved psoriasis severity. Conversely, probiotic supplementation increased antioxidant capacity and decreased inflammatory markers. Consider keeping a food diary to identify your personal triggers.
Can essential oils help psoriasis?
Tea tree oil (Melaleuca alternifolia) shows anti-inflammatory potential due to its terpinen-4-ol content. A systematic review of RCTs identified terpinen-4-ol as the major component with anti-inflammatory properties. However, the same review noted higher quality trials are needed specifically for psoriasis. Other essential oils lack sufficient clinical evidence for psoriasis specifically. Always dilute essential oils properly before skin application. Common side effects include skin irritation and potential allergic sensitization. Test on a small area first.
Does diet affect psoriasis?
Yes, diet affects psoriasis through its impact on systemic inflammation and the gut microbiome. Omega-3 fatty acid supplementation produced significant PASI score reductions in a meta-analysis of 10 RCTs with 560 participants. The gut-skin axis connects dietary choices to skin inflammation. Probiotic supplementation improved both PASI scores and quality-of-life measures, with decreased inflammatory markers and increased antioxidant capacity. An anti-inflammatory diet rich in fish, vegetables, and fermented foods may support symptom management.
How long does psoriasis remission last?
Psoriasis remission duration varies significantly between individuals, ranging from weeks to years. No research establishes an average remission length because of this variability. Factors influencing remission include treatment adherence, trigger avoidance, stress management, and individual disease characteristics. In one probiotic RCT, improved responses persisted at six-month follow-up with lower relapse rates in the treatment group. Consistent use of evidence-based natural remedies combined with lifestyle modifications may help extend remission periods, though outcomes cannot be guaranteed.
Can psoriasis be cured naturally?
No, psoriasis cannot be cured naturally or by any other means. It is a chronic autoimmune condition. Natural remedies offer symptom management and may extend remission periods, but they do not cure the underlying disease. A 2025 systematic review of 20 RCTs with 1,115 patients concluded that herbal therapies show therapeutic benefit for psoriasis management, but additional rigorous research is needed. Claims of 'permanent natural cures' are not supported by scientific evidence. Focus on evidence-based management strategies combining natural remedies with medical care as appropriate.
What are the best oils for psoriasis?
Based on clinical evidence, omega-3 fish oil (EPA/DHA) taken orally shows the strongest evidence, with a meta-analysis of 10 RCTs demonstrating significant PASI improvements. For topical use, tea tree oil contains terpinen-4-ol with anti-inflammatory properties, though psoriasis-specific RCTs are limited. Coconut oil and other emollient oils help moisturize and reduce scaling but lack specific psoriasis RCT evidence. Indigo naturalis oil extract containing indirubin showed 56.3% PASI 75 response at 8 weeks in a dose-controlled trial.
Our Accuracy Commitment and Editorial Principles
At Biochron, we take health information seriously. Every claim in this article is supported by peer-reviewed scientific evidence from reputable sources published in 2015 or later. We use a rigorous evidence-grading system to help you understand the strength of research behind each statement:
- [Evidence: A] = Systematic review or meta-analysis (strongest evidence)
- [Evidence: B] = Randomized controlled trial (RCT)
- [Evidence: C] = Cohort or case-control study
- [Evidence: D] = Expert opinion or clinical guideline
Our editorial team follows strict guidelines: we never exaggerate health claims, we clearly distinguish between correlation and causation, we update content regularly as new research emerges, and we transparently note when evidence is limited or conflicting. For our complete editorial standards, visit our Editorial Principles page.
This article is for informational purposes only and does not constitute medical advice. Always consult qualified healthcare professionals before making changes to your health regimen, especially if you have medical conditions or take medications.
References
- 1 . Efficacy and safety of curcumin in psoriasis: preclinical and clinical evidence and possible mechanisms, Frontiers in Pharmacology, 2022, Zhang S et al. PubMed [Evidence: A]
- 2 . Effect of Vitamin D Supplementation on Psoriasis Severity in Patients With Lower-Range Serum 25-Hydroxyvitamin D Levels: A Randomized Clinical Trial, JAMA Dermatology, 2023, Jenssen M et al. PubMed [Evidence: B]
- 3 . Psoriasis and Vitamin D: A Systematic Review and Meta-Analysis, Nutrients, 2023, Formisano E et al. PubMed [Evidence: A]
- 4 . Efficacy of ω-3 supplementation in patients with psoriasis: a meta-analysis of randomized controlled trials, Clinical Rheumatology, 2019, Clark CCT et al. PubMed [Evidence: A]
- 5 . Probiotic supplementation improves clinical outcomes and quality of life indicators in patients with plaque psoriasis: A randomized double-blind clinical trial, Clinical Nutrition ESPEN, 2021, Moludi J et al. PubMed [Evidence: B]
- 6 . Comparison of indirubin concentrations in indigo naturalis ointment for psoriasis treatment: a randomized, double-blind, dosage-controlled trial, British Journal of Dermatology, 2018, Lin YK et al. PubMed [Evidence: B]
- 7 . Herbal medicine for treating psoriasis: A systematic review, Complementary Therapies in Medicine, 2025, Anheyer M et al. PubMed [Evidence: A]
- 8 . Efficacy of an adjuvant Lactobacillus rhamnosus formula in improving skin lesions as assessed by PASI in patients with plaque psoriasis, Archives of Dermatological Research, 2023, Suriano ES et al. PubMed [Evidence: B]
- 9 . Efficacy of probiotic supplementation in the treatment of psoriasis-A systematic review and meta-analysis, Journal of Cosmetic Dermatology, 2024, Wei K et al. PubMed [Evidence: A]
- 10 . Patient-reported outcomes of curcumin supplementation in rheumatoid arthritis and psoriatic arthritis: a cross-sectional survey, Rheumatology International, 2024, Purohit R et al. PubMed [Evidence: D]
- 11 . Efficacy and Safety of Oral Administration of a Mixture of Probiotic Strains in Patients with Psoriasis: A Randomized Controlled Clinical Trial, Acta Dermato-Venereologica, 2019, Navarro-López V et al. PubMed [Evidence: B]
- 12 . Curcumin and Curcuma longa Extract in the Treatment of 10 Types of Autoimmune Diseases: A Systematic Review and Meta-Analysis of 31 Randomized Controlled Trials, Frontiers in Immunology, 2022, Zeng L et al. PubMed [Evidence: A]
- 13 . Safety of dermatologic medications in pregnancy and lactation: An update - Part I: Pregnancy, Journal of the American Academy of Dermatology, 2024, McMullan P et al. PubMed [Evidence: D]
- 14 . Topical Botanical Agents for the Treatment of Psoriasis: A Systematic Review, American Journal of Clinical Dermatology, 2017, Farahnik B et al. PubMed [Evidence: A]
- 15 . Efficacy and safety of Melaleuca alternifolia (tea tree) oil for human health—A systematic review of randomized controlled trials, Frontiers in Pharmacology, 2023, Kairey L et al. PubMed [Evidence: A]
Medical Disclaimer
This content is for informational and educational purposes only. It is not intended to provide medical advice or to take the place of such advice or treatment from a personal physician. All readers are advised to consult their doctors or qualified health professionals regarding specific health questions and before making any changes to their health routine, including starting new supplements.
Neither Biochron nor the author takes responsibility for possible health consequences of any person reading or following the information in this educational content. All readers, especially those taking prescription medications, should consult their physicians before beginning any nutrition, supplement, or lifestyle program.
If you have a medical emergency, call your doctor or emergency services immediately.






