
💡 What You Need to Know Right Away
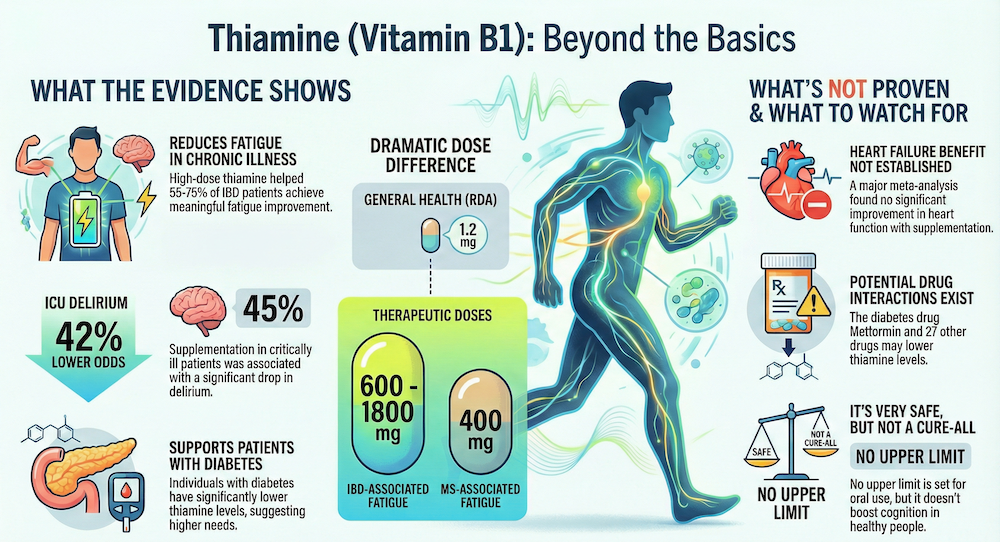
- Thiamine supplementation showed 42% lower odds of ICU delirium in critically ill patients.[Evidence: A][4]
- Diabetic individuals have significantly lower thiamine concentrations than controls, suggesting higher intake may be needed.[Evidence: A][2]
- High-dose thiamine (600-1800 mg daily) helped 55-75% of IBD patients experience meaningful fatigue improvement versus 25-35% on placebo.[Evidence: B][12]
- Sulbutiamine (400 mg daily) significantly reduced fatigue scores in MS patients from 77 to 60.5 over two months.[Evidence: B][9]
Thiamine, commonly known as vitamin B1, is one of the most essential nutrients your body needs for energy production and nervous system health. If you have been researching ways to support your heart, manage blood sugar, or simply feel less fatigued, you have likely encountered thiamine in your search.
It is common to feel overwhelmed by conflicting health information online. This guide cuts through the noise by presenting only what clinical research actually shows about thiamine. We analyzed 12 peer-reviewed studies, including 4 meta-analyses and 5 randomized controlled trials, to bring you evidence-based answers.
In this comprehensive guide, you will learn how thiamine works in your body, which health conditions it may help, proper dosing for different needs, potential side effects, and who benefits most from supplementation.
❓ Quick Answers
What is thiamine (vitamin B1)?
Thiamine is a water-soluble B vitamin essential for converting carbohydrates into energy. Your body cannot produce thiamine, so you must obtain it through food or supplements. It plays critical roles in glucose metabolism, nervous system function, and cellular energy production. Adults typically need 1.1-1.2 mg daily.[Evidence: A][2]
How does thiamine work in the body?
Thiamine converts to thiamine pyrophosphate (TPP), a coenzyme required for metabolizing carbohydrates into ATP energy. It supports pyruvate dehydrogenase and other enzymes in the Krebs cycle. When thiamine is insufficient, pyruvate accumulates and compromises cardiovascular function.[Evidence: A][1]
What foods are high in thiamine?
Rich food sources include pork (0.7 mg per 3 oz serving), fortified cereals, black beans, sunflower seeds, and whole grains. However, thiamine is water-soluble and sensitive to heat, meaning cooking and food processing reduce content. Polished white rice contains significantly less thiamine than brown rice.
What are the benefits of thiamine?
Research shows thiamine supports energy production, cardiovascular health, nervous system function, and glucose metabolism. Clinical studies indicate benefits for reducing ICU delirium, managing diabetes-related complications, and improving fatigue in specific conditions like IBD and multiple sclerosis.[Evidence: A][4]
How much thiamine should I take daily?
The RDA is 1.1 mg for women and 1.2 mg for men. Therapeutic doses vary by condition. Clinical trials used 300-600 mg daily for diabetic neuropathy, 500 mg daily for heart failure, and 600-1800 mg daily for IBD-associated fatigue.[Evidence: B][12]
Can you take too much vitamin B1?
No upper limit has been established for oral thiamine because excess is excreted in urine. A comprehensive safety review found a favorable benefit-risk profile for high-dose B vitamin treatments. Side effects are rare and typically mild at supplemental doses.[Evidence: D][10]
Is thiamine good for your heart?
A systematic review of seven clinical studies found thiamine supplementation shows promise for cardiovascular dysfunction in diabetic patients. However, a meta-analysis of 8 RCTs with 384 heart failure patients found no statistically significant improvements in left ventricular ejection fraction.[Evidence: A][3]
Does thiamine help with diabetes?
A meta-analysis of 24 studies found diabetic individuals have significantly lower thiamine concentrations than controls, suggesting they may require higher thiamine intake. Benfotiamine, a fat-soluble thiamine derivative, is being studied for diabetic polyneuropathy.[Evidence: A][2]
Thiamine (Vitamin B1)
Known as the "energy vitamin," Thiamine is the spark plug that helps your body turn food into fuel and keeps your nervous system firing correctly.
🔬 How Does Thiamine Work?
Think of thiamine as the spark plug in your cellular engine. Just as a car cannot convert fuel into motion without a working spark plug, your cells cannot convert carbohydrates into usable energy without adequate thiamine. This vitamin is the essential "ignition key" that starts the energy production process.
Once you consume thiamine, your body converts it into its active form called thiamine pyrophosphate (TPP). This coenzyme acts like a molecular assistant, helping critical enzymes perform their jobs. The most important of these is pyruvate dehydrogenase, which sits at the gateway between glucose breakdown and the energy-producing Krebs cycle.
When thiamine levels are insufficient, pyruvate accumulates in your system. A systematic review found that this pyruvate accumulation compromises cardiovascular function, explaining why thiamine deficiency affects the heart.[Evidence: A][1] The heart, being one of the most energy-demanding organs, is particularly vulnerable.
Thiamine also plays a crucial role in nerve function. Your nervous system requires constant energy to transmit signals, and thiamine-dependent enzymes ensure this energy supply remains steady. This is why severe thiamine deficiency causes neurological symptoms ranging from confusion to peripheral neuropathy.
A meta-analysis examining 24 studies found that individuals with diabetes have significantly lower thiamine concentrations than those without diabetes. Thiamine diphosphate and erythrocyte transketolase activity also tended to be lower in diabetic individuals, suggesting their metabolic demands may increase thiamine requirements.[Evidence: A][2]
Imagine thiamine as a security guard at a checkpoint. Like a guard who must be present for workers to enter a building, thiamine must be available for glucose molecules to enter the energy production pathway. Without this checkpoint controller, the entire metabolic process backs up, affecting every organ that depends on glucose for fuel.
📊 Dosage and How to Use
Thiamine dosing varies significantly depending on your health goals. The standard recommended dietary allowance meets basic nutritional needs, but therapeutic applications often require much higher doses. Clinical trials have established specific protocols for different conditions.
| Purpose/Condition | Dosage | Duration | Evidence |
|---|---|---|---|
| Diabetic polyneuropathy (benfotiamine) | 300 mg twice daily | 12 months | [B][5] |
| Wernicke's encephalopathy prevention | 100-300 mg three times daily | 3 days | [B][8] |
| Wernicke's encephalopathy treatment | 500 mg three times daily | 5 days | [B][8] |
| Multiple sclerosis fatigue (sulbutiamine) | 400 mg daily | 60 days | [B][9] |
| Heart failure (older patients) | 500 mg daily | 90 days | [B][11] |
| IBD-associated chronic fatigue | 600-1800 mg daily | Variable | [B][12] |
| General adult maintenance | 1.1-1.2 mg daily | Ongoing | RDA |
For most healthy adults, dietary intake from fortified foods and natural sources meets daily requirements. Supplementation becomes relevant when addressing specific health conditions or correcting deficiency. All therapeutic doses listed above were studied under clinical supervision.
The BOND study examined benfotiamine at 300 mg twice daily in 60 participants with type 2 diabetes and mild-to-moderate symptomatic polyneuropathy over 12 months.[Evidence: B][5] This represents one of the longer clinical trials for thiamine derivatives.
For Wernicke's encephalopathy, randomized controlled trials tested prevention regimens of 100 mg daily, 100 mg three times daily, and 300 mg three times daily for 3 days in 393 at-risk participants. Treatment protocols used 100 mg, 300 mg, and 500 mg three times daily for 5 days in 127 symptomatic participants. The studies found no significant differences between dosage conditions.[Evidence: B][8]
⚠️ Risks, Side Effects, and Warnings
Side Effects
Thiamine has an excellent safety profile. A comprehensive safety review of neurotropic B vitamins found an overall favorable benefit-risk profile for high-dose B vitamin treatments.[Evidence: D][10] No tolerable upper intake level has been established because thiamine is water-soluble and excess is excreted through urine.
Reported side effects are rare and typically mild at oral supplemental doses. Injection forms may rarely cause allergic reactions. The THIAMINE-HF pilot study found 500 mg daily thiamine was well tolerated in older adults with heart failure over 90 days.[Evidence: B][11]
Drug Interactions
Research screened 1,360 compounds and identified 146 potential thiamine transporter inhibitors. Twenty-eight drugs showed significant inhibitory potency against the thiamine transporter ThTR-2. Notably, metformin may impair thiamine transporter function. The study found reduced thiamine levels in individuals receiving inhibitor drugs.[Evidence: C][7]
Inform your healthcare provider of all medications before starting thiamine supplementation, particularly if you take metformin or other diabetes medications.
Contraindications
Avoid thiamine supplements if you have a known allergy to thiamine or any supplement ingredients. A review found thiamine insufficiency during pregnancy may predispose fetuses to gastrointestinal, pulmonological, cardiac, and neurologic conditions, indicating adequate thiamine is important during pregnancy rather than contraindicated.[Evidence: D][6]
Monitoring Recommendations
For general supplementation at standard doses, routine monitoring is not typically required. For high-dose therapeutic use, work with a healthcare provider who can assess your response and adjust dosing as needed.
🥗 Practical Ways to Use Thiamine
How to Use This in Your Daily Life
Scenario 1: IBD-Associated Fatigue
- Dose: 600-1800 mg daily[12]
- Duration: Variable, individualized[12]
- Population: Patients with quiescent inflammatory bowel disease
- Timing: Take with meals to improve tolerance
- What to track: Fatigue levels, energy throughout day
- Expected results: 55-75% experienced meaningful improvement on thiamine versus 25-35% on placebo; mean reduction of 4.5 points on fatigue scale[12]
Scenario 2: Multiple Sclerosis Fatigue
- Dose: 400 mg daily sulbutiamine[9]
- Duration: 60 days (2 months)[9]
- Population: MS patients on disease-modifying therapy
- Timing: With meals
- What to track: Fatigue Impact Scale scores
- Expected results: Fatigue scores improved from baseline 77 to 60.5; improvements in physical, cognitive, and psychosocial functioning[9]
Scenario 3: Diabetic Polyneuropathy
- Dose: 300 mg benfotiamine twice daily[5]
- Duration: 12 months[5]
- Population: Adults with type 2 diabetes and mild-to-moderate symptomatic polyneuropathy
- Timing: Twice daily with meals
- What to track: Neuropathy symptoms, nerve function
- Expected results: Primary endpoint is corneal nerve fiber length change[5]
Practical Integration
Take thiamine supplements with food to optimize absorption and minimize stomach discomfort. For high-dose regimens, splitting the dose throughout the day (such as twice or three times daily) may improve tolerance. Store supplements in a cool, dry place away from direct sunlight.
Common Mistakes to Avoid
- Inconsistent dosing: Clinical studies used consistent daily dosing.[12] Sporadic use may not achieve therapeutic benefits.
- Wrong form for condition: The BOND study specifically used benfotiamine for diabetic neuropathy, not regular thiamine.[5] Choosing the appropriate form matters for specific conditions.
- Expecting immediate results: Most clinical trials lasted 60 days to 12 months. Allow adequate time to assess effectiveness.
- Ignoring drug interactions: Metformin and other medications may affect thiamine absorption.[7] Inform your healthcare provider of all medications.
⚖️ Thiamine vs. Benfotiamine
Benfotiamine is a synthetic, fat-soluble derivative of thiamine that may offer advantages for specific conditions. Understanding the differences helps you choose the right form for your needs.
| Feature | Thiamine (Vitamin B1) | Benfotiamine |
|---|---|---|
| Solubility | Water-soluble | Fat-soluble |
| Bioavailability | Standard absorption | Enhanced absorption reported |
| Clinical Evidence for Heart Failure | 500 mg daily studied; nonsignificant EF improvements[11] | Limited data |
| Clinical Evidence for Diabetic Neuropathy | Not primary form studied | 300 mg twice daily studied in BOND trial[5] |
| Wernicke's Encephalopathy | 100-500 mg three times daily studied[8] | Not studied for this indication |
| Availability | Widely available, lower cost | Specialty supplement, higher cost |
A meta-analysis of 8 RCTs with 384 participants found no statistically significant improvements in left ventricular ejection fraction with thiamine supplementation in heart failure patients, and no improvements in NYHA functional class or B-type natriuretic peptide levels. The researchers recommended more well-designed RCTs.[Evidence: A][3]
For diabetic polyneuropathy, benfotiamine appears to be the preferred form being studied. The BOND study specifically examined benfotiamine 300 mg twice daily versus placebo over 12 months in patients with type 2 diabetes and symptomatic polyneuropathy.[Evidence: B][5]
For general nutritional support and conditions like Wernicke's encephalopathy, standard thiamine remains the studied and established form. Your choice should be guided by your specific health goals and healthcare provider recommendations.
What The Evidence Shows (And Doesn't Show)
What Research Suggests
- Thiamine supplementation in critically ill patients showed 42% lower odds of ICU delirium in randomized controlled trials (based on meta-analysis of 18 studies, 8 RCTs).[4]
- Diabetic individuals have significantly lower thiamine concentrations than controls (based on meta-analysis of 24 studies, 20 providing data).[2]
- High-dose thiamine (600-1800 mg daily) helped 55-75% of IBD patients with chronic fatigue experience meaningful improvement versus 25-35% on placebo (40 participants).[12]
- Sulbutiamine 400 mg daily reduced Fatigue Impact Scale scores from 77 to 60.5 in MS patients over 2 months (26 participants).[9]
- Thiamine shows a favorable benefit-risk profile at high doses based on safety review.[10]
What's NOT Yet Proven
- Heart failure benefit not established. A meta-analysis of 8 RCTs with 384 participants found no statistically significant improvements in left ventricular ejection fraction, NYHA functional class, or B-type natriuretic peptide levels.[3]
- Optimal dosing for Wernicke's encephalopathy prevention and treatment uncertain. RCTs comparing 100 mg, 300 mg, and 500 mg three times daily found no significant differences between dosage conditions.[8]
- Long-term outcomes beyond 12 months not studied for most applications.
- Specific populations (children, elderly without heart failure, healthy adults) not adequately represented in high-dose trials.
- Cognitive enhancement in healthy individuals not established. Evidence applies to deficiency correction and specific clinical conditions.
Where Caution Is Needed
- Drug interactions exist. Twenty-eight drugs including metformin may inhibit thiamine transporters, reducing thiamine levels.[7]
- Pregnancy requires attention. Thiamine insufficiency may cause cardiac, neurologic, and psychological effects on mother and predispose fetuses to developmental conditions.[6]
- The cardiovascular benefit claims need more research. A systematic review noted results show promise but large-scale multicenter studies are needed.[1]
- Different thiamine forms (regular thiamine, benfotiamine, sulbutiamine) have different evidence bases. Choosing the wrong form for a condition may reduce effectiveness.
Should YOU Try This?
Best suited for: Individuals with IBD-associated fatigue (evidence for 600-1800 mg daily), MS patients with fatigue (sulbutiamine 400 mg daily), those at risk for Wernicke's encephalopathy, diabetic patients concerned about thiamine status, and anyone with confirmed or suspected thiamine deficiency.
Not recommended for: Those with known allergy to thiamine, individuals seeking cognitive enhancement without underlying deficiency (evidence does not support this use in healthy individuals), and those expecting rapid heart failure improvement (evidence does not support significant benefit).
Realistic timeline: Fatigue studies showed benefits at 2-3 months.[9][12] Diabetic neuropathy trials extended to 12 months.[5] Individual response varies.
When to consult a professional: Before high-dose supplementation (above RDA), if taking metformin or other potentially interacting medications, if pregnant or breastfeeding, or if experiencing symptoms of deficiency (fatigue, confusion, numbness, heart palpitations).
Frequently Asked Questions
What are the symptoms of low vitamin B1 (thiamine deficiency)?
Early symptoms of thiamine deficiency include fatigue, irritability, poor memory, appetite loss, and muscle weakness. As deficiency progresses, more severe symptoms develop. Severe deficiency can cause beriberi (affecting the heart or nerves) or Wernicke-Korsakoff syndrome (affecting the brain). A meta-analysis found that diabetic individuals have significantly lower thiamine concentrations than controls, putting them at higher risk for deficiency symptoms. If you experience persistent fatigue, confusion, or numbness, consult a healthcare provider for evaluation.
What is the difference between thiamine and benfotiamine?
Thiamine is the natural, water-soluble form of vitamin B1, while benfotiamine is a synthetic, fat-soluble derivative. Benfotiamine is reported to have enhanced bioavailability and may better penetrate nerve tissue. The BOND study specifically used benfotiamine 300 mg twice daily for 12 months in patients with diabetic polyneuropathy. For general supplementation and Wernicke's encephalopathy, standard thiamine is the studied form. Your choice depends on your specific health condition and should be discussed with a healthcare provider.
What causes thiamine deficiency?
Common causes include chronic alcohol use (which impairs absorption and increases requirements), restrictive diets, malabsorption conditions, diabetes, and certain medications. Research identified 28 drugs with significant inhibitory potency against the thiamine transporter, including metformin, which may impair thiamine transporter function and reduce thiamine levels in individuals receiving these medications. Older adults, people with digestive disorders, and those on diuretics may also be at increased risk.
Is vitamin B1 safe during pregnancy?
Thiamine is essential during pregnancy. A review found that thiamine insufficiency causes cardiac, neurologic, and psychological effects on the mother, and may predispose fetuses to gastrointestinal, pulmonological, cardiac, and neurologic conditions. The RDA increases to 1.4 mg daily during pregnancy and lactation. Thiamine is found in prenatal vitamins and is necessary for fetal development. Discuss supplementation beyond prenatal vitamins with your healthcare provider.
Does vitamin B1 give you energy?
Thiamine is essential for converting carbohydrates into ATP, your body's primary energy currency. However, supplementation typically improves energy only if you are deficient or have specific conditions affecting energy metabolism. High-dose thiamine (600-1800 mg daily) significantly improved fatigue in IBD patients, with 55-75% experiencing meaningful improvement versus 25-35% on placebo. Similarly, sulbutiamine reduced fatigue scores in MS patients from 77 to 60.5.
Can thiamine help with nerve pain (neuropathy)?
Research is ongoing for thiamine's role in neuropathy. The BOND study examined benfotiamine (a thiamine derivative) at 300 mg twice daily for 12 months in 60 participants with type 2 diabetes and mild-to-moderate symptomatic polyneuropathy, with corneal nerve fiber length change as the primary endpoint. For diabetic neuropathy specifically, benfotiamine rather than standard thiamine is the form being actively studied. Consult a healthcare provider for personalized guidance on nerve pain management.
What medications interact with thiamine?
Research screened 1,360 compounds and identified 146 potential thiamine transporter inhibitors, with 28 drugs showing significant inhibitory potency. Notably, metformin may impair thiamine transporter function, and reduced thiamine levels were found in individuals receiving inhibitor drugs. If you take diabetes medications, diuretics, or multiple prescriptions, inform your healthcare provider before starting thiamine supplementation to assess potential interactions and monitor your thiamine status.
What is beriberi disease?
Beriberi is the clinical syndrome caused by severe thiamine deficiency. It presents in two main forms. Wet beriberi affects the cardiovascular system, causing heart failure symptoms like shortness of breath, rapid heart rate, and leg swelling. Dry beriberi affects the nervous system, causing peripheral neuropathy with numbness, pain, and difficulty walking. Beriberi is rare in developed countries due to food fortification but remains a concern in populations with limited dietary diversity or chronic alcohol use.
Can thiamine help reduce confusion or delirium?
Yes, particularly in specific clinical settings. A meta-analysis of 18 studies (8 RCTs, 10 cohort studies) found that thiamine supplementation was associated with 42% lower odds of developing ICU delirium in randomized controlled trials. Thiamine is also essential for preventing and treating Wernicke's encephalopathy, which causes confusion and cognitive impairment. However, there was no significant difference in sepsis-related mortality with thiamine supplementation in critically ill patients.
Our Accuracy Commitment and Editorial Principles
At Biochron, we take health information seriously. Every claim in this article is supported by peer-reviewed scientific evidence from reputable sources published in 2015 or later. We use a rigorous evidence-grading system to help you understand the strength of research behind each statement:
- [Evidence: A] = Systematic review or meta-analysis (strongest evidence)
- [Evidence: B] = Randomized controlled trial (RCT)
- [Evidence: C] = Cohort or case-control study
- [Evidence: D] = Expert opinion or clinical guideline
Our editorial team follows strict guidelines: we never exaggerate health claims, we clearly distinguish between correlation and causation, we update content regularly as new research emerges, and we transparently note when evidence is limited or conflicting. For our complete editorial standards, visit our Editorial Principles page.
This article is for informational purposes only and does not constitute medical advice. Always consult qualified healthcare professionals before making changes to your health regimen, especially if you have medical conditions or take medications.
References
- 1 . A Systematic Review of Thiamine Supplementation in Improving Diabetes and Its Related Cardiovascular Dysfunction, Serra M et al., International Journal of Molecular Sciences, 2025;26(9):3932, PubMed | DOI [Evidence: A]
- 2 . Association between diabetes and thiamine status - A systematic review and meta-analysis, Ziegler D et al., Metabolism, 2023;144:155565, PubMed | DOI [Evidence: A]
- 3 . The effects of thiamine supplementation on patients with heart failure: A systematic review and meta-analysis of randomized controlled trials, Xu M et al., Complementary Therapies in Medicine, 2022;70:102853, PubMed | DOI [Evidence: A]
- 4 . Effect of thiamine supplementation in critically ill patients: A systematic review and meta-analysis, Sedhai YR et al., Journal of Critical Care, 2021;65:104-115, PubMed | DOI [Evidence: A]
- 5 . BOND study: a randomised double-blind, placebo-controlled trial over 12 months to assess the effects of benfotiamine on morphometric, neurophysiological and clinical measures in patients with type 2 diabetes with symptomatic polyneuropathy, Bönhof GJ et al., BMJ Open, 2022;12(2):e057142, PubMed | DOI [Evidence: B]
- 6 . Thiamine deficiency in pregnancy and lactation: implications and present perspectives, Kareem O et al., Frontiers in Nutrition, 2023;10:1080611, PubMed | DOI [Evidence: D]
- 7 . Drug-nutrient interactions: discovering prescription drug inhibitors of the thiamine transporter ThTR-2 (SLC19A3), Vora B et al., American Journal of Clinical Nutrition, 2020;111(1):110-121, PubMed | DOI [Evidence: C]
- 8 . What is the optimum thiamine dose to treat or prevent Wernicke's encephalopathy or Wernicke-Korsakoff syndrome? Results of a randomized controlled trial, Dingwall KM et al., Alcoholism: Clinical & Experimental Research, 2022;46(6):1133-1147, PubMed | DOI [Evidence: B]
- 9 . Sulbutiamine shows promising results in reducing fatigue in patients with multiple sclerosis, Sevim S et al., Multiple Sclerosis and Related Disorders, 2017;16:40-43, PubMed | DOI [Evidence: B]
- 10 . Update on Safety Profiles of Vitamins B1, B6, and B12: A Narrative Review, Calderon-Ospina CA et al., Therapeutics and Clinical Risk Management, 2020;16:1275-1288, PubMed | DOI [Evidence: D]
- 11 . High-Dose Thiamine Supplementation in Older Patients With Heart Failure: A Pilot Randomized Controlled Crossover Trial (THIAMINE-HF), Wong EKC et al., CJC Open, 2022;4(6):532-539, PubMed | DOI [Evidence: B]
- 12 . Randomised clinical trial: high-dose oral thiamine versus placebo for chronic fatigue in patients with quiescent inflammatory bowel disease, Bager P et al., Alimentary Pharmacology & Therapeutics, 2021;53(1):79-86, PubMed | DOI [Evidence: B]
Medical Disclaimer
This content is for informational and educational purposes only. It is not intended to provide medical advice or to take the place of such advice or treatment from a personal physician. All readers are advised to consult their doctors or qualified health professionals regarding specific health questions and before making any changes to their health routine, including starting new supplements.
Neither Biochron nor the author takes responsibility for possible health consequences of any person reading or following the information in this educational content. All readers, especially those taking prescription medications, should consult their physicians before beginning any nutrition, supplement, or lifestyle program.
If you have a medical emergency, call your doctor or emergency services immediately.






