
💡 What You Need to Know Right Away
A copper blood test is a blood test that measures the amount of copper in your blood to detect Wilson disease, Menkes disease, copper toxicity, and nutritional deficiencies. Most copper in your blood is carried by a protein called ceruloplasmin, and abnormal levels can indicate serious health problems affecting your liver, brain, and nervous system.
Also known as: Serum Copper Test, Total Copper Blood Test, Plasma Copper Test, Copper Serum or Plasma
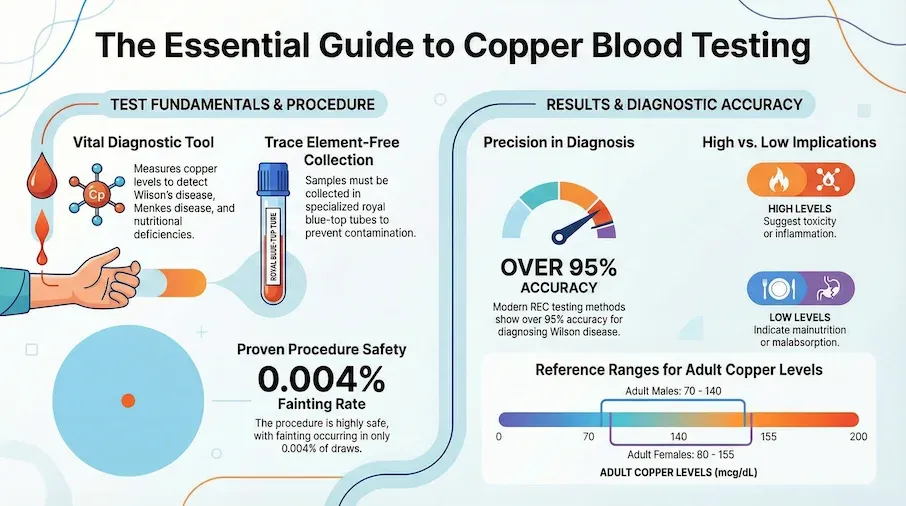
- Correctly identifies Wilson disease in about 8 to 10 out of 10 cases when using ceruloplasmin measurement[Evidence: A][10]
- Newer testing methods (REC) show over 95% accuracy for diagnosing Wilson disease[Evidence: A][1]
- Normal adult range is 70-155 mcg/dL, with slight variations by age and gender[Evidence: A][2]
- Very safe procedure. Fainting occurs in only about 4 out of 100,000 blood draws[Evidence: C][11]
If your doctor has ordered a copper blood test, you might be wondering what it means and what to expect. It's normal to feel uncertain when facing any medical test, especially one you may not have heard of before.
Copper is an essential mineral your body needs in small amounts. It helps build strong bones, supports your immune system, and keeps your nerves working properly. But too much or too little copper can cause serious health problems. A copper blood test helps your doctor check whether your copper levels are in a healthy range.
This guide explains everything you need to know about the copper blood test, including why your doctor might order it, how it's done, what the results mean, and when you should be concerned. We'll also cover what makes this test different from the ceruloplasmin test and help you understand your next steps after getting results.
❓ Quick Answers
What is a copper blood test?
A copper blood test measures the total amount of copper in your blood serum or plasma. Copper is an essential trace mineral that your body needs for normal growth, bone health, immune function, and neurological development. The test helps diagnose conditions where copper levels are abnormally high or low, including Wilson disease and Menkes disease.
What is a copper blood test used for?
Doctors order this test to diagnose Wilson disease, a genetic condition where copper builds up in your liver and brain[Evidence: A][2]. It also helps diagnose Menkes disease in infants, assess copper deficiency from malnutrition or malabsorption, and detect copper toxicity from environmental or dietary exposure.
Do I need to fast for a copper blood test?
Most labs do not require fasting for a copper blood test. However, some specialty labs prefer a 12-hour fast to improve accuracy. Check with your specific testing facility before your appointment, as protocols vary between laboratories[Evidence: D][3].
What is the normal range for a copper blood test?
Normal copper levels for adults are 70-140 mcg/dL for males and 80-155 mcg/dL for females. Children and pregnant women have different reference ranges. People with Wilson disease typically show average ceruloplasmin levels around 50 mg/L, compared to about 290 mg/L in healthy individuals[Evidence: C][7].
How is a copper blood test done?
A healthcare professional draws blood from a vein in your arm using a needle. The sample is collected in a special royal blue-top tube that is trace element-free to prevent contamination. The entire blood draw takes about 2-5 minutes. Results are typically available within 2-4 days[Evidence: C][11].
Is a copper blood test safe for kids?
Yes, the copper blood test is safe for children of all ages, including infants. In children being tested for Wilson disease, specialized pediatric thresholds improve accuracy, with ceruloplasmin correctly identifying the condition in over 95 out of 100 cases[Evidence: C][8]. Parents can request experienced pediatric phlebotomists to help children feel more comfortable.
How long does it take to get copper blood test results?
Standard copper blood test results are typically available within 2-4 days. Specialty tests like Relative Exchangeable Copper (REC) may take 5-7 days. Your doctor will contact you when results are ready, or you may access them through a patient portal[Evidence: C][6].
What is the difference between copper and ceruloplasmin tests?
The copper test measures total copper in your blood, while the ceruloplasmin test measures the protein that carries most of your blood copper. Doctors often order both tests together. Research shows ceruloplasmin correctly identifies Wilson disease in about 8 to 10 out of 10 cases[Evidence: A][10].
Copper Blood Test
Copper is an essential mineral for nerve health, bone growth, and collagen production. This test measures the amount of copper in your blood to help diagnose Wilson's disease, monitor nutritional deficiencies, and evaluate liver health.
🔬 How Does Copper Testing Work?
To understand your copper blood test results, it helps to know how copper works in your body. Think of copper as a construction foreman overseeing multiple building projects at once. Just as a foreman coordinates workers across different sites, copper coordinates essential processes throughout your body, including building red blood cells, maintaining nerve health, and supporting your immune system.
When you eat foods containing copper, your intestines absorb it and send it to your liver. Your liver then attaches copper to a protein called ceruloplasmin, which acts like a delivery truck, carrying copper to tissues that need it. About 65-90% of the copper in your blood travels bound to ceruloplasmin.
The copper blood test measures all copper in your blood, both the copper bound to ceruloplasmin and the small amount of "free" copper circulating independently. In people with Wilson disease, the standard copper test correctly identifies the condition in about 6 out of 10 cases[Evidence: A][2]. This is why doctors often combine it with ceruloplasmin testing for better accuracy.
Newer Testing Methods
Recent advances have improved copper testing accuracy. A newer measurement called Relative Exchangeable Copper (REC) acts like a more precise thermometer. Rather than just measuring total copper, it specifically identifies the copper that can cause harm when elevated. Research shows this newer test correctly identified Wilson disease in over 95 out of 100 cases[Evidence: A][1] and correctly ruled it out in over 99 out of 100 cases[Evidence: A][1].
In people with sudden severe liver failure, studies suggest combined copper-liver enzyme scores correctly classified Wilson disease in over 99 out of 100 cases[Evidence: B][5]. These newer methods represent significant improvements over traditional testing, though they may not be available at all laboratories.
Clinical guidelines from 2025 now recommend using the REC measurement along with the Leipzig scoring system to diagnose Wilson disease[Evidence: D][3].
🧪 What to Expect: The Real User Experience
During the Blood Draw
When you arrive for your copper blood test, a healthcare worker called a phlebotomist will ask you to sit in a chair or lie on an exam table. They'll wrap a tourniquet around your upper arm, which feels similar to a blood pressure cuff squeeze and lasts about 30-60 seconds while they locate your vein.
Before the needle insertion, you'll feel an alcohol swab on your skin. It feels cold and wet but evaporates quickly. The needle insertion itself causes a sharp pinch or sting lasting 1-2 seconds, followed by a dull ache or pressure sensation while the blood is collected (typically 30-90 seconds). The actual blood collection takes only 2-5 minutes from start to finish.
The blood is collected in a special royal blue-top tube that is trace element-free. This prevents contamination that could affect your results.
What You'll Feel After
After the needle is removed, the phlebotomist applies light pressure with a cotton ball or gauze. You may notice mild soreness at the puncture site for a few hours, similar to a minor bruise. In a large-scale analysis of nearly 680,000 blood draws, fainting occurred in only about 4 out of 100,000 procedures[Evidence: C][11].
A small bruise (typically dime-sized) may appear at the puncture site, showing yellow-green discoloration that resolves within 3-5 days. This is completely normal and does not indicate any problem with your test.
How to Make It Easier
- Eat a light meal beforehand: Having food in your system 1-2 hours before reduces lightheadedness risk
- Stay hydrated: Drink water the day before. It makes veins easier to find and reduces needle repositioning
- Wear short sleeves: Easier arm access reduces anxiety from rolling up tight sleeves
- Look away from the needle: Focus on the wall, ceiling, or conversation with the phlebotomist if you're squeamish
- Practice slow, deep breathing: Inhale for 4 counts, exhale for 6 counts to reduce anxiety
- Tell them if you faint easily: The phlebotomist can have you lie down instead of sitting
For Children and Infants
- Bring a comfort item: A stuffed animal, blanket, or favorite toy provides distraction
- Hold your infant: Parent touch during the procedure reduces crying
- Ask about numbing cream: Available at some labs. Apply 30-60 minutes before the draw
- Explain simply: Tell older children what will happen using age-appropriate language
- Plan a reward: A sticker or small treat afterward creates positive association for future tests
📊 Preparation and Procedure
Before Your Test
Preparation for a copper blood test is straightforward. Most laboratories do not require fasting, though some specialty labs prefer a 12-hour fast. Always confirm requirements with your specific testing facility. Inform your healthcare provider about all medications you take, as some can affect copper levels.
Reference Ranges
| Population | Normal Range (mcg/dL) | Notes |
|---|---|---|
| Adult Males | 70-140 | Standard reference range |
| Adult Females | 80-155 | Slightly higher than males |
| Pregnancy | Elevated | Copper levels naturally rise during pregnancy |
| Children (Ceruloplasmin) | 16.8 mg/dL cutoff | Pediatric threshold for Wilson disease screening[Evidence: C][8] |
Test Components Often Ordered Together
| Test | What It Measures | Turnaround Time | Evidence |
|---|---|---|---|
| Serum Copper (CPT 82525) | Total copper in blood | 2-4 days | [A][2] |
| Ceruloplasmin (CPT 82390) | Copper-carrying protein | 2-4 days | [A][10] |
| 24-Hour Urine Copper (CPT 84156) | Copper excreted over 24 hours | 3-5 days | [C][6] |
| Relative Exchangeable Copper (REC) | Bioavailable copper percentage | 5-7 days | [A][1] |
Understanding Your Results
High Copper Levels May Indicate
- Wilson disease (when ceruloplasmin is also low)
- Acute or chronic inflammation
- Copper toxicity from environmental exposure
- Certain liver diseases
- Pregnancy (normal elevation)
Low Copper Levels May Indicate
- Menkes disease (rare genetic condition)
- Copper deficiency from malnutrition
- Malabsorption conditions
- Excessive zinc supplementation
- Gastric bypass surgery complications
⚠️ Risks, Side Effects, and Safety
The copper blood test is a routine blood draw with minimal risks. The test itself is painless beyond the brief needle insertion, though you may feel a short pinch when the needle enters your vein.
Risk Factors for Complications
Research shows that having more than 5 tubes of blood drawn increases fainting risk by about 8 times[Evidence: C][11]. Waiting more than 15 minutes before the blood draw increases fainting risk by about 4 times[Evidence: C][11]. If you have a history of fainting during blood draws, inform the phlebotomist so you can lie down during the procedure.
Contraindications
- Active cellulitis at puncture site: Blood draw should be performed at a different location
- AV fistula in arm: Dialysis patients should have blood drawn from the other arm
- Severe coagulopathy: Patients with very low platelet counts (<50,000) may need additional precautions
It's normal to feel anxious about medical tests, but most people tolerate blood draws well. The entire procedure takes only 2-5 minutes, and the brief discomfort is over quickly.
🥗 Practical Ways to Prepare and Follow Up
How to Prepare for Your Test
- Check fasting requirements: Call your lab 24 hours before to confirm whether fasting is needed
- List your medications: Bring a list of all medications, including supplements like zinc (which affects copper levels)
- Schedule morning appointments: Labs are less crowded early, reducing wait times and anxiety
- Wear comfortable clothing: Short sleeves or loose-fitting tops make arm access easier
- Stay hydrated: Drink plenty of water the day before to make veins easier to locate
What Happens After Your Test
If Your Results Are Normal
Normal results mean your copper levels fall within the healthy reference range for your age and gender. Your doctor may recommend routine monitoring if you have risk factors for copper metabolism disorders. No immediate follow-up testing is typically needed.
If Your Copper Is High
Your doctor will likely order additional tests, including ceruloplasmin and 24-hour urine copper collection. Clinical guidelines recommend using multiple markers together for diagnosis[Evidence: D][3]. If Wilson disease is suspected, you may need a liver biopsy to measure hepatic copper content, genetic testing for ATP7B mutations, or an eye exam to look for Kayser-Fleischer rings.
If Your Copper Is Low
Low copper triggers investigation for nutritional deficiencies, malabsorption conditions, or genetic disorders. In infants, Menkes disease testing includes plasma catecholamine analysis. Your doctor will discuss appropriate follow-up based on your specific situation and symptoms.
Factors That Can Affect Results
- Estrogen/oral contraceptives: Can increase copper levels
- Zinc supplements: Can decrease copper levels
- Antacids: May decrease copper absorption
- Pregnancy: Naturally increases copper levels
- Inflammation/infection: Can temporarily increase copper levels
What to Look for When Choosing a Copper Blood Test Provider
The quality of your test results depends on the laboratory and healthcare provider. Here's what to consider when selecting where to have your copper blood test performed:
Lab Quality Markers
- CLIA certification: Clinical Laboratory Improvement Amendments (CLIA) accreditation is required for all US clinical laboratories Why it matters: Federal quality standards ensure accurate results
- CAP accreditation: College of American Pathologists certification represents a higher standard than CLIA alone Why it matters: Rigorous proficiency testing and inspections
- Trace element testing capabilities: Labs must use special trace element-free (royal blue-top) collection tubes Why it matters: Standard tubes can contaminate samples and give inaccurate results
- Turnaround time: Standard results in 2-4 days. Specialty tests (REC) may take 5-7 days Why it matters: Faster results enable quicker treatment decisions
Questions to Ask Your Provider
- Do you use trace element-free collection tubes for copper testing?
- Do I need to fast before this test? (Protocols vary by lab)
- When will my results be available?
- Will my doctor contact me, or should I check a patient portal?
- Is this test covered by my insurance?
- Do you offer newer tests like Relative Exchangeable Copper (REC)?
Red Flags
- No CLIA certification: Unlicensed labs lack quality oversight
- Using standard collection tubes: Copper testing requires special trace element-free tubes
- Unusually cheap pricing: May indicate unaccredited lab or inadequate quality controls
- No clear turnaround time: Professional labs can provide specific timelines
Copper Blood Test vs Ceruloplasmin Test: What's the Difference?
The copper blood test and ceruloplasmin test measure different things but are often ordered together. The copper test measures total copper in your blood, while the ceruloplasmin test measures the protein that carries most of your blood copper. Understanding both results together gives your doctor a more complete picture of your copper metabolism.
| Feature | Copper Blood Test | Ceruloplasmin Test |
|---|---|---|
| What It Measures | Total copper in serum or plasma | Copper-carrying protein levels |
| CPT Code | 82525 | 82390 |
| Sensitivity for Wilson Disease | 61.5%[Evidence: A][2] | 77-99%[Evidence: A][10] |
| Specificity for Wilson Disease | 99.1%[Evidence: A][2] | 56-83%[Evidence: A][10] |
| When to Use | Initial screening, copper toxicity assessment | Wilson disease diagnosis, inflammation assessment |
| Turnaround Time | 2-4 days | 2-4 days |
When Doctors Order Both Tests
Research shows combining multiple tests improves diagnostic accuracy. In people being tested for Wilson disease, combining ceruloplasmin with 24-hour urine copper correctly ruled out the condition in all non-Wilson cases[Evidence: C][9]. Finding Kayser-Fleischer rings during an eye exam correctly identified Wilson disease in about 8 out of 10 cases with no false positives[Evidence: C][9].
Newer Combined Approaches
The Relative Exchangeable Copper (REC) test combines the advantages of both traditional tests. In people newly diagnosed with suspected Wilson disease, research shows the REC test correctly identified the condition in all cases tested[Evidence: A][2]. This newer test is becoming more widely available at specialty laboratories.
What The Evidence Shows (And Doesn't Show)
What Research Suggests
- The newer REC biomarker correctly identifies Wilson disease in over 95 out of 100 cases and rules it out in over 99 out of 100 cases (validated in over 700 people)[Evidence: A][1]
- Ceruloplasmin testing correctly identifies Wilson disease in about 8 to 10 out of 10 cases across multiple studies (over 5,600 participants analyzed)[Evidence: A][10]
- Combined testing (ceruloplasmin plus urine copper) correctly ruled out Wilson disease in all non-Wilson cases tested[Evidence: C][9]
- In acute liver failure, copper-based biomarkers show excellent diagnostic performance for identifying Wilson disease[Evidence: B][4]
- Blood draw is extremely safe, with fainting occurring in only 0.004% of procedures (27 events in nearly 680,000 draws)[Evidence: C][11]
What's NOT Yet Proven
- Optimal diagnostic thresholds vary between studies. Ceruloplasmin cutoffs range from 150-200 mg/L in adults and 16.8 mg/dL in children, with different sensitivity/specificity tradeoffs
- Long-term monitoring protocols for treated Wilson disease patients are not fully standardized
- REC testing availability is limited. Not all laboratories offer this newer biomarker
- Pediatric-specific reference ranges for newer biomarkers like REC have not been established in large studies
- The impact of various medications on copper test results requires further systematic study
Where Caution Is Needed
- Standard copper testing alone has only about 62% sensitivity for Wilson disease. Multiple tests are needed for accurate diagnosis[Evidence: A][2]
- Copper levels rise naturally during pregnancy and inflammation, which can complicate interpretation
- Specimen contamination from improper collection tubes can cause falsely elevated results. Confirm your lab uses trace element-free (royal blue-top) tubes
- Self-diagnosis based on results is not recommended. Always consult your healthcare provider for interpretation
Should YOU Get This Test?
Best suited for: People with unexplained liver disease, neurological symptoms of unknown cause, family history of Wilson disease or Menkes disease, suspected copper deficiency, or unexplained anemia with neurological symptoms
Not recommended for: Routine health screening without specific indications. Copper testing is not part of standard wellness panels
Realistic timeline: Results typically available in 2-4 days for standard tests. Specialty tests may take 5-7 days. Diagnosis of copper disorders often requires multiple tests over several weeks
When to consult a professional: If you have symptoms of Wilson disease (liver problems, tremors, difficulty speaking), family history of copper disorders, or unexplained anemia with neurological symptoms, discuss testing with your doctor
Frequently Asked Questions
What causes high copper levels in the blood?
High copper levels can result from Wilson disease, acute or chronic liver disease, inflammation, infection, or environmental copper exposure. Pregnancy naturally increases copper levels. Certain medications including estrogen and oral contraceptives can also elevate copper. In people with Wilson disease, average ceruloplasmin levels are around 50 mg/L, compared to about 290 mg/L in healthy individuals. Your doctor will consider your complete medical history when interpreting elevated results.
What causes low copper levels in the blood?
Low copper levels may indicate Menkes disease (a rare genetic condition in infants), copper deficiency from inadequate dietary intake, malabsorption conditions like celiac disease or Crohn's disease, excessive zinc supplementation (which competes with copper absorption), or complications from gastric bypass surgery. In children being tested for copper deficiency, specialized pediatric reference ranges apply.
Can I take my regular medications before the copper blood test?
Continue taking your prescription medications unless your doctor specifically instructs otherwise. However, let your healthcare provider know about all medications and supplements you take, especially zinc supplements, estrogen, oral contraceptives, and antacids, as these can affect copper levels. Bring a list of all your medications to your appointment so the lab can note any potential interferences.
How accurate is the copper blood test for diagnosing Wilson disease?
The accuracy depends on which tests are used. Research shows the standard copper test alone correctly identifies Wilson disease in about 6 out of 10 cases. Ceruloplasmin correctly identifies Wilson disease in about 8 to 10 out of 10 cases. The newer REC test shows over 95% accuracy. Combining multiple tests provides the most reliable diagnosis.
What is the 24-hour urine copper test, and when is it needed?
The 24-hour urine copper test measures how much copper your body excretes in your urine over a full day. You collect all urine in a special container for 24 hours. In children being tested for Wilson disease, 24-hour urine copper above 70 micrograms correctly identified the condition in about 8 out of 10 cases. Doctors typically order this test when blood copper or ceruloplasmin results suggest a possible copper metabolism disorder.
How is Wilson disease treated if my test is positive?
Wilson disease is treated with medications that remove excess copper from your body (chelation therapy). Clinical guidelines recommend medications like penicillamine or trientine. Treatment is lifelong but highly effective when started early. Your doctor will monitor your copper levels regularly to ensure treatment is working. A low-copper diet may also be recommended alongside medication.
At what age should children be tested for copper disorders?
Testing age depends on the suspected condition. Menkes disease testing should occur in the first weeks of life when treatment can be most effective. Wilson disease typically presents in children ages 5-35, though symptoms may appear earlier. In pediatric populations, specific ceruloplasmin cutoffs apply. A threshold of 16.8 mg/dL showed excellent diagnostic performance, correctly identifying Wilson disease in over 95 out of 100 cases.
Can copper levels be affected by diet?
Yes, dietary factors can influence copper levels. Copper-rich foods include shellfish, nuts, seeds, organ meats, and chocolate. Excessive zinc intake (often from supplements) can decrease copper absorption. However, for diagnostic purposes, a single meal typically does not significantly affect test results. Your doctor will consider your overall nutritional status when interpreting results. People with confirmed copper disorders may need to follow specific dietary restrictions.
Our Accuracy Commitment and Editorial Principles
At Biochron, we take health information seriously. Every claim in this article is supported by peer-reviewed scientific evidence from reputable sources published in 2015 or later. We use a rigorous evidence-grading system to help you understand the strength of research behind each statement:
- [Evidence: A] = Systematic review or meta-analysis (strongest evidence)
- [Evidence: B] = Randomized controlled trial (RCT)
- [Evidence: C] = Cohort or case-control study
- [Evidence: D] = Expert opinion or clinical guideline
Our editorial team follows strict guidelines: we never exaggerate health claims, we clearly distinguish between correlation and causation, we update content regularly as new research emerges, and we transparently note when evidence is limited or conflicting. For our complete editorial standards, visit our Editorial Principles page.
This article is for informational purposes only and does not constitute medical advice. Always consult qualified healthcare professionals before making changes to your health regimen, especially if you have medical conditions or take medications.
References
- 1 . Relative exchangeable copper: A highly specific and sensitive biomarker for Wilson disease diagnosis, JHEP Reports, 2025, Djebrani-Oussedik N, et al. PubMed [Evidence: A]
- 2 . Relative Exchangeable Copper, Exchangeable Copper and Total Copper in the Diagnosis of Wilson Disease, Liver International, 2025, Lorenzen C, et al. PubMed [Evidence: A]
- 3 . EASL-ERN Clinical Practice Guidelines on Wilson's disease, Journal of Hepatology, 2025, European Association for the Study of the Liver. PubMed [Evidence: D]
- 4 . Performance of Relative Exchangeable Copper for the Diagnosis of Wilson Disease in Acute Liver Failure, Journal of Inherited Metabolic Disease, 2025, Spirea D, et al. PubMed [Evidence: B]
- 5 . Diagnosing Wilson Disease in Acute Liver Failure: Comparison of Existing and Experimental Biomarkers, American Journal of Gastroenterology, 2025, Sandahl TD, et al. PubMed [Evidence: B]
- 6 . Urinary 24-hour copper excretion at the time of diagnosis in children with Wilson's disease, Acta Gastro-Enterologica Belgica, 2018, Aksu AÜ, et al. PubMed [Evidence: C]
- 7 . The optimal threshold of serum ceruloplasmin in the diagnosis of Wilson's disease: A large hospital-based study, PLoS One, 2018, Xu R, et al. PubMed [Evidence: C]
- 8 . Assessment of the diagnostic value of serum ceruloplasmin for Wilson's disease in children, BMC Gastroenterology, 2022, Lu X, et al. PubMed [Evidence: C]
- 9 . Efficacy of Different Diagnostic Test for Identifying Wilson's Disease, Mymensingh Medical Journal, 2022, Sonia ZF, et al. PubMed [Evidence: C]
- 10 . Biomarkers for diagnosis of Wilson's disease, Cochrane Database of Systematic Reviews, 2019, Ryan A, et al. PubMed [Evidence: A]
- 11 . Analysis of vasovagal syncope in the blood collection room in patients undergoing phlebotomy, Scientific Reports, 2020, Yoshimoto A, et al. PubMed [Evidence: C]
Medical Disclaimer
This content is for informational and educational purposes only. It is not intended to provide medical advice or to take the place of such advice or treatment from a personal physician. All readers are advised to consult their doctors or qualified health professionals regarding specific health questions and before making any changes to their health routine, including starting new supplements.
Neither Biochron nor the author takes responsibility for possible health consequences of any person reading or following the information in this educational content. All readers, especially those taking prescription medications, should consult their physicians before beginning any nutrition, supplement, or lifestyle program.
If you have a medical emergency, call your doctor or emergency services immediately.






